Soft tissue calcifications



Clinical History
Young man, 20 years old with intense myoarticular pain mostly at muscles insertions and limited range of motion (active and passive) of the limbs.
Imaging Findings
On physical examination presented semi-flexion position of the arms and legs with joint stiffness, skin darkened patches, hair loss, burning pain and symmetric skin hardening in the upper and lower limbs (figures 1 and 2). -Personal background: Hemolytic Uremic Syndrome at 19 years old with cerebral ischemic involvement (documented by contrast enhanced MRI), due to 19 gene mutation with factor H deficiency. Chronic renal failure on hemodialysis. -Laboratory tests: hypercalcemia; Normal PTH, TRAP, CPK and aldolase. Negative FAN, anti-ADN, anti-SCL70 and latex. ACE within normal values and ESR 36 mm/h. CT examination was performed (figures 3 to 9).
Discussion
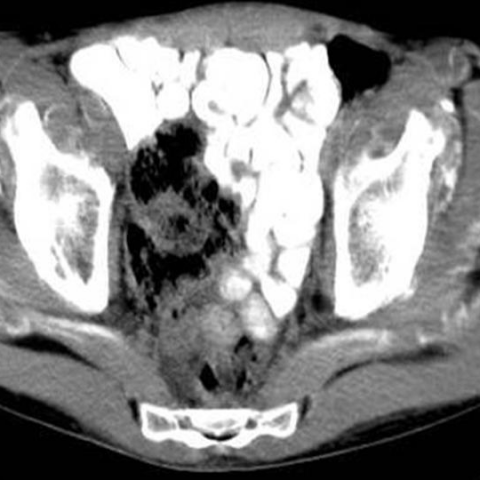
There are linear and confluent calcifications in soft tissues of extremities, paraspinal muscles and psoas with flexion contractures and evidence of renal disease manifested as thinning of renal parenchyma. A skin biopsy was performed (figure 10).
First identified in 1997, Nephrogenic Systemic Fibrosis (NSF) has been reported only in patients with acute or chronic severe renal insufficiency or patients with renal dysfunction due to the hepato-renal syndrome. Since the description of NSF (previously labeled nephrogenic fibrosing dermopathy) more than 200 patients have been reported. Patients with this condition develop fibrosis of the skin and connective tissues throughout their body. The face is typically spared. The skin thickening may inhibit flexion and extension of joints resulting in contractures. In addition, patients may develop widespread fibrosis of other organs.
A skin biopsy is necessary to confirm the diagnosis. The condition may be debilitating or cause death often from sepsis as a complication of immobility or from hypoventilation if lung and diaphragm involvement occurs. Its cause is unknown and there is no consistently successful treatment. Improvement has been reported following recovery of renal function, either spontaneously, after renal transplantation, or with immunomodulatory treatments including extracorporeal photophoresis and phototherapy
Histologically, skin lesions demonstrate dermal thickening with deep penetration of
collagen bundles into the superficial fascia. Staining for dermal mucin is positive. Dermal cells expressing CD34 support the concept of a bone marrow–derived “circulating fibrocyte” playing a pathogenic role. A combination of pathologic and laboratory features distinguishes NSF from similar conditions, including systemic sclerosis, scleromyxoedema, and eosinophilic vasculitis. These features include the absence of anti-scl70 and anticentromere antibodies, as well as normal serum electrophoresis. Vascular disease, thrombotic events, chronic liver disease, and the presence of antiphospholipid antibodies have been associated with NSF although not implicated in its pathogenesis.
Since 1998, the increasing use of gadolinium-enhanced magnetic resonance imaging in the established renal failure population (ERF) to avoid exposure to iodinated contrast material or as pretransplantation investigation parallels the description of patients with NSF. Collidge et al.1 found a positive association between gadolinium-based contrast agent administration and development of NSF in the ERF population, as well as a positive association between cumulative dose of gadodiamide used and dosing events. It is mandatory for every radiologist to become familiar with this entity to avoid putting susceptible populations at risk.
Differential Diagnosis List
Final Diagnosis
Nephrogenic Systemic Fibrosis (NSF)
Liscense
Figures
Physical examination

Skin lesions

CT

Skin biopsy. HE histology.

CT 1

CT 2

CT 3

CT 4

CT 5
CT 6

Medical Imaging Analysis Report
I. Imaging Findings
The patient is a 20-year-old young male with severe muscle and joint pain, primarily at the sites where muscles attach, accompanied by restricted range of motion (both active and passive) in the limbs. Based on the provided CT and related images, the following key findings are observed:
- Linear or confluent calcifications in the soft tissues (including the limbs, paraspinal muscle groups, and the psoas major region), covering a wide area.
- Involvement of muscles, fascia, and subcutaneous tissue, with some areas showing thickening or calcium deposits in the soft tissues, correlating with imaging findings typically suggesting fibrosis and calcification.
- Thinning of the renal parenchyma, indicating possible chronic renal dysfunction.
- Some degree of flexion contracture observed in the limb joints, indicating contracture or fibrosis of soft tissues and tendons.
- Skin pathology slides (shown) reveal thickening of the dermis, abnormal distribution of collagen fiber bundles extending into the superficial fascia, and mucin deposition in the dermis.
II. Potential Diagnoses
Considering the clinical symptoms (muscle-joint stiffness, pain, restricted mobility), imaging findings (widespread soft tissue fibrosis or calcification), skin biopsy results (fibrosis and mucin deposition in the dermis and superficial fascia), and the background of renal insufficiency, the following diagnoses or differential diagnoses should be considered:
- Nephrogenic Systemic Fibrosis (NSF)
Cause: More common in patients with severe acute or chronic renal insufficiency, potentially associated with exposure to gadolinium-based contrast agents. Clinical and pathological features include skin thickening, contractures, and possible visceral involvement. Skin biopsy may show dermal and fascial fibrosis, increased CD34-positive cells, and mucin deposition. - Systemic Sclerosis (Scleroderma)
Cause: A type of connective tissue disease that can present with skin thickening and joint contractures, but it is often accompanied by immunological markers (such as anti-Scl-70 or anticentromere antibodies), and facial involvement is common. - Calcium Pyrophosphate Deposition Disease (e.g., Pseudogout) or Calcific Tendinitis
Cause: In chronic renal failure, generalized disorders of calcium-phosphorus metabolism may occur, but they usually do not present with such marked fibrosis and deep tissue involvement. - Scleroderma-like Calcinosis Cutis
Cause: May be seen in connective tissue diseases or metabolic abnormalities, primarily presenting with cutaneous or subcutaneous calcifications, but large-scale contractures and pronounced deep fascial fibrosis, as in this case, are less common.
III. Most Likely Final Diagnosis
For this patient:
- Multiple areas of soft tissue fibrosis and calcification involving the limbs, trunk, psoas major, and paraspinal muscle groups.
- Clear evidence of renal impairment (thinning of the renal parenchyma).
- Skin biopsy results consistent with collagen proliferation and mucin deposition in the dermis and superficial fascia, with no indication of specific autoantibodies (such as anti-Scl-70 or anticentromere antibodies).
- Clinically, progressive restriction of joint mobility and contractures.
Based on these features, the most likely final diagnosis is “Nephrogenic Systemic Fibrosis (NSF).”
IV. Treatment Plan and Rehabilitation
1. Treatment Strategies
- Improve or restore renal function: If possible, actively treat the underlying renal disease (including dialysis, kidney transplantation, etc.) to help alleviate systemic symptoms.
- Avoid or use gadolinium contrast agents with caution: For patients with renal insufficiency, strictly evaluate the risks of gadolinium-based contrast agents, considering alternative imaging methods when necessary.
- Immunomodulatory treatment: Some patients may attempt treatment with corticosteroids, immunosuppressants, photopheresis (e.g., extracorporeal photopheresis), or UV light therapy, although efficacy is not fully established.
- Supportive treatment: Including pain control, nutritional support, and maintenance of joint mobility.
2. Rehabilitation and Exercise Prescription
The goal of rehabilitation is to reduce joint and soft tissue contractures, maintain muscle strength and function, and improve quality of life. A gradual exercise principle (FITT-VP) should be applied, based on the patient’s condition, renal function, cardiopulmonary function, and tolerance to therapy.
- Frequency (F): Start with 2–3 sessions per week. Depending on tolerance, gradually increase to 3–5 sessions per week.
- Intensity (I):
- Low-to-moderate intensity is appropriate, avoiding excessive exercise that could cause fatigue or soft tissue injury.
- Simple range-of-motion exercises (e.g., flexion, extension, lifts) can be used, supplemented by isometric or low-load resistance training.
- Time (T): Start each session at 15–30 minutes, and gradually increase based on adaptability, avoiding overexertion.
- Type (T):
- Early stages focus on joint mobilization, passive stretching, and gentle muscle strengthening exercises.
- After symptom improvement, introduce simple aerobic exercises (e.g., brisk walking on flat ground, stationary cycling).
- Progression (P): Increase exercise duration or slightly increase resistance as symptoms improve and exercise tolerance grows, with a focus on small increments.
- Volume & Individualization (V – Volume & P – Pattern/Individualization):
- Consider the patient’s level of pain and range-of-motion limitations. Weekly aerobic exercise should not exceed 90–150 minutes, and resistance training intensity should be adjusted according to muscle strength evaluations.
- Continuously assess renal function and electrolyte balance. If significant edema, fatigue, or increased joint pain occurs, adjust the rehabilitation plan promptly.
For this patient, the main priority is to prevent new soft tissue injuries and further loss of joint mobility. A thorough assessment and warm-up should be performed before starting rehabilitation training to reduce pain and minimize the risk of injury caused by contractures and adhesions.
Safety Considerations: As the patient has renal insufficiency, particular attention should be paid to fluid and electrolyte balance after exercise, avoiding high-intensity workouts, and closely monitoring the progression of joint and skin lesions.
Disclaimer:
This report provides a reference-based medical analysis derived from the materials provided and is not a substitute for an in-person consultation or a professional doctor’s diagnosis and treatment plan. If you have any doubts or your condition worsens, it is recommended that you seek prompt medical attention from a specialized hospital department.
Human Doctor Final Diagnosis
Nephrogenic Systemic Fibrosis (NSF)