Osteoid osteoma of the femur: CT-guided percutaneous radiofrequency ablation



Clinical History
A 27 year old male was referred to our department with 7 months history of lasting left thigh pain.
Imaging Findings
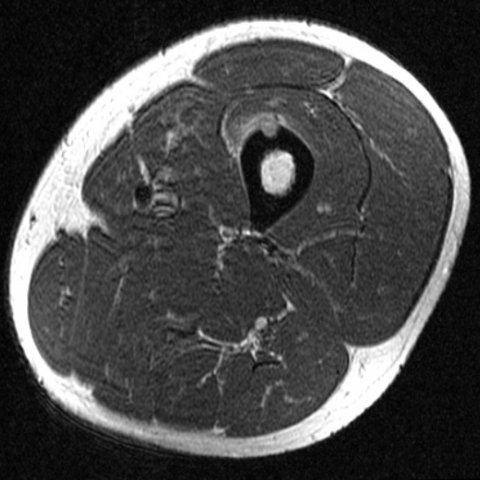
A 27 year old man was referred to our department for persistent pain in the region of the left quadriceps muscle with onset 7 months before; symptoms worsened at night interfering with sleep and receded completely following low-dose NSAID administration. An ultrasound (US) examination was performed, showing an 8-mm nodule-shaped irregularity of the cortex of the middle portion of the left femural diaphysis, without any significant alteration of the surrounding soft tissues. Subsequently, an MRI examination was performed showing an intracortical nodule characterized by low signal intensity relative to muscle on T1-weighted images with iso/hypointensity on T2-weighted images. Oedema of the quadriceps muscle adjacent to the lesion was apparent on STIR images, while after intravenous administration of paramagnetic contrast material, marked, early, and steady enhancement of the central part of the nodule (called the nidus) was detected, consistent with the diagnosis of osteoid osteoma. CT-guided percutaneous radiofrequency ablation (RFA) of the lesion was planned. Preliminary diagnostic CT scan for lesion localization confirmed the osteolytic structure of the osteoid osteoma, containing a small calcified core corresponding to the nidus. The RFA procedure was carried out under patient sedation through an 18-gauge probe with rectractable hooks, delivering RF energy inside the lesion for four minutes at target temperature. After treatment, complete and stable remission of pain was obtained. A control US examination performed ten days later showed bone scarring with minimal perilesional hematoma.
Discussion
Osteoid osteoma (OO) is a usually small (typically less than 2cm), benign neoplasm of the bone, characterized pathologically by a central portion named nidus. It occurs more frequently in male adolescents and young adults, and its predilected sites are the appendicular skeleton (especially the femur) and, more rarely, the axial skeleton. When long bones are affected, OO usually has a metaphyseal or diaphyseal location, while the epiphyses are less frequently involved. Diagnosis is suggested by clinical findings and is confirmed by imaging modalities such as conventional X-ray, CT, and MRI. OO often requires ablation due to the intense continuous pain that it may cause, which usually persists during night, increases following alcohol intake, and tends to recede after NSAID administration. RFA is a relatively novel technique for mini-invasive treatment of OO, representing a valid and safer alternative to surgery with fewer complications. Patients’ recovery after RFA is complete and almost immediate with substantially lower costs compared with traditional surgical therapy.
Differential Diagnosis List
Final Diagnosis
Osteoid osteoma treated with CT-guided RFA.
Liscense
Figures
Pretreatment US examination.

Pretreatment MRI.




Preprocedural CT.


CT-guided RFA.


Post-treatment US examination.

1. Imaging Findings
Based on the provided imaging (ultrasound, MRI, CT, etc.), the following findings are noted:
- Lesion location: In the left femoral shaft or near the diaphyseal-metaphyseal region (depending on the patient’s actual imaging), with slight reactive changes in the local soft tissue.
- Appearance and density/signal: On CT, a relatively small (usually < 2cm) low-density “nidus” can be observed, surrounded by sclerotic bone; on T2-weighted MRI, there may be a marked edema zone around the area. On ultrasound, a localized cortical bulge or heterogeneous echo may be seen, as well as mild soft tissue edema.
- Typical characteristics: On CT, the center of the “nidus” often appears as a low-density or calcified focus with obvious surrounding sclerosis; MRI shows focal bone marrow and soft tissue edema, aligning with the clinical presentation of persistent pain.
- Soft tissue changes: There may be mild inflammatory reaction or soft tissue edema, with no obvious abscess or large-scale invasion.
2. Possible Diagnoses
Based on the patient’s clinical history (persistent pain that worsens at night and responds well to NSAIDs) and imaging features (a bone lesion smaller than 2cm with a typical “nidus” on CT), the main considerations for diagnosis and differential diagnosis include:
- Osteoid Osteoma: Common in adolescents and young adults. Typical symptoms include nocturnal pain effectively relieved by non-steroidal anti-inflammatory drugs (NSAIDs). CT typically shows a small “nidus” with surrounding sclerotic bone, matching the clinical and imaging findings in this case.
- Stress Fracture: Often appears in weight-bearing bones or after excessive exercise. On CT or MRI, a linear discontinuity of the cortex or bone marrow edema may be seen, but they often lack the characteristic “nidus.”
- Osteomyelitis/ Infection: Can present with bone destruction and soft tissue abscess. Clinically, inflammatory markers are often elevated, and imaging typically shows a less localized lesion than a small “nidus,” with more extensive surrounding changes.
- Benign Bone Tumors or Tumor-like Lesions (e.g., Osteochondroma, Bone Cyst): Generally differ in shape, location, and signal characteristics compared to osteoid osteoma. They also often lack the classic nocturnal pain pattern.
3. Final Diagnosis
Taking into account:
- Patient characteristics: 27-year-old male with significant nocturnal pain, relieved by regular NSAIDs.
- Imaging findings: A bone cortical lesion on CT, less than 2 cm, with a typical “nidus” and surrounding sclerosis.
- Pain features and related history: 7-month duration, worsens at night, pain aggravated by alcohol, consistent with osteoid osteoma.
Overall, the most likely diagnosis is: Osteoid Osteoma.
4. Treatment Plan and Rehabilitation
4.1 Treatment Strategies
- Anti-inflammatory and Analgesic Medications: Such as NSAIDs, used to control pain and reduce inflammation, especially effective for nocturnal pain.
- Radiofrequency Ablation (RFA): The first choice for minimally invasive treatment. Under CT guidance, radiofrequency ablation can destroy the lesion with minimal trauma and rapid recovery.
- Surgical Curettage or Resection: Should the lesion location be unsuitable for RFA, or if recurrence or residual disease occurs after RFA, surgical intervention may be considered.
4.2 Rehabilitation and Exercise Prescription
After treatment, a gradual, individualized rehabilitation exercise program should be adopted according to the patient’s condition. General recommendations are as follows:
- Acute Phase (1–2 weeks post-operation):
- Protective weight-bearing or use of crutches to reduce stress on the affected limb and avoid excessive activity.
- Light range of motion (ROM) exercises (e.g., ankle pumps, knee flexion-extension) to prevent joint stiffness.
- Upper limb strength training and core stabilization exercises can be done in seated or supine positions for safety.
- Recovery Phase (2–6 weeks post-operation):
- Gradually increase weight-bearing on the affected limb, transitioning to simple functional training in a standing position (such as standing balance, mild squats).
- Begin moderate aerobic exercise (e.g., using a stationary bike with support, swimming), gradually increasing session time to 15–20 minutes, 3–4 times per week.
- Continue with ROM and flexibility exercises such as seated leg raises and stretching.
- Strengthening Phase (6 weeks post-operation and onward):
- Once bone healing progresses well, focus on strengthening lower limb muscles by gradually adding resistance exercises (resistance bands, weight training).
- Extend aerobic exercise to 20–30 minutes per session, 3–5 times per week, increasing intensity in stages.
- If recovery is satisfactory, under guidance from a specialist or physical therapist, gradually return to running, ball sports, or other high-impact activities, while monitoring pain and load tolerance.
The entire rehabilitation process should follow the FITT-VP principles (Frequency, Intensity, Time, Type, Volume, and Progression) and be adjusted according to postoperative recovery and bone healing status.
If the patient has other comorbidities (e.g., osteoporosis, poor cardiopulmonary function), more conservative approaches in exercise intensity and type are needed, with regular imaging follow-up to evaluate bone healing.
Disclaimer
This report is based on the available imaging and clinical history, and only serves as a reference. It does not replace a face-to-face clinical diagnosis or professional medical advice. If you have any questions or if your condition changes, please consult an orthopedic surgeon, radiologist, or the relevant specialist promptly.
Human Doctor Final Diagnosis
Osteoid osteoma treated with CT-guided RFA.