Mandibular Osteonecrosis Associated with Biphosphonate Therapy


Clinical History
A 76 years old man presented with pain and swelling of the left mandibular region initiated after a dental extraction 3 months ago. Clinical history comprises prostate cancer without any osteoblastic bony metastasis and treatment with intravenous bisphosphonates for 3 years.
Imaging Findings
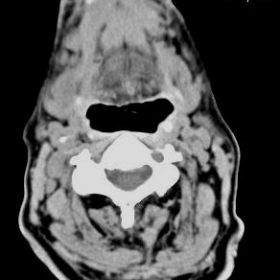
The patient presented with pain and swelling of the left mandibular region initiated after a dental extraction 3 months ago. There was no response to the antibiotic treatment. The patient was also under treatment with intravenous administration zoledronic acid for the last three years. The intraoral exploration revealed no healing extraction sockets and partially exposed adjacent alveolar bone. Soft tissue swelling, subcutaneous fat oedema and local skin thickening also noted.
The middle part and the region of the mental protuberance of the lower mandible show erosion of the anterior surface of the bone with soft tissue involvement and the presence of sequestration within it.
The histological examination of the lesion revealed the presence of bone necrosis, inflammatory granulation tissue and abscess formation.
These results were indicative of biphosphonate-related-osteonecrosis (BRON) and the patient initiated an antibiotic treatment in combination with non-steroid anti-inflammatories and oral antiseptic solutions whereas medication with biphosphonates was interrupted.
Discussion
Bisphosphonates are synthetic analogs of pyrophosphate. They inhibit osteoclastic action, have an anti-angiogenetic effect, and are helpful in the maintenance of the calcium and phosphate equilibrium. Accumulating data show that these drugs are useful in diseases with propensities toward osseous metastases. In particular, they are effective in diseases in which there is clear up-regulation of osteoclastic or osteolytic activity such as breast cancer, multiple myeloma and Paget’s disease, as well as to prevent the osteoporosis in the menopause. Despite the fact that osseous metastases in prostate cancer manifest as osteosclerosis rather than osteolysis, studies show that bisphosphonates are useful in the management of this disease. In particular, they have demonstrated an impact on osteoporosis associated with hormonal therapy, bone pain from metastases, and skeleton-related events from prostatic adenocarcinoma.
Adverse effects associated with the use of bisphosphonates are infrequent and consist of pyrexia, renal function impairment, hypocalcemia and avascular osteonecrosis of the jaw (ONJ). ONJ was initially associated with the use of zoledronic acid but occurrences after pamidronate use have also been reported after a long period of exposure.
BRON is an exclusive affection of the jaws related to smaller bone traumas with a deficient healing and vascular compromise caused by bisphosphonate contained in the usual microbiological flora of the oral cavity.
Recently, there have been established 3 characteristics that must be present to pone the diagnosis of BRON: (i) current or previous treatment with a bisphosphonate, (ii) exposed, necrotic bone in the maxillofacial region that has persisted for more than 8 weeks and (iii) no history of radiation therapy of the jaws. The main risk factor for this complication is the previous history of dento-alveolar surgery, but it may appear spontaneously in cases without previous trauma
Osteonecrosis refers to the death of the bone as a result of impaired blood supply to the affected areas. Cancer and its treatment have been described as risk factors for the development of osteonecrosis. The most common site of osteonecrosis is the femoral head. Avascular ONJ has been associated predominantly with radiation of the head and neck, known as osteoradionecrosis, but has also been described after chemotherapy. Recently, ONJ has been reported after treatment with the bisphosphonates pamidronate and zoledronic acid in cancer patients. Apart from bisphosphonates, corticosteroids and chemotherapy can also be implicated in the development of ONJ. ONJ is a complication that is correlated with long-term use of bisphosphonates.
Differential Diagnosis List
Final Diagnosis
Mandibular Osteonecrosis Associated with Biphosphonate Therapy
Liscense
Figures
Neck CT


Neck CT


1. Imaging Findings
Based on the provided head and neck CT images, local bony changes can be observed in the left mandible, specifically:
- Discontinuity of the bony structure in certain areas of the left mandible; suspected sequestrum (i.e., abnormally high-density or “white bone-like” regions on imaging, with partially unclear demarcation from the surrounding bone).
- Accompanying signs of swelling or thickening in the adjacent soft tissue, suggesting local inflammation or tissue reaction.
- No clear large-scale fracture line is noted, but there may be small-scale bone destruction or collapse.
- Increased density in the adjacent soft tissue, indicating possible infection or inflammatory changes.
Overall imaging features suggest long-standing unhealed bone destruction of the mandible and possible sequestrum formation. Considering the patient’s medical history, ischemic necrosis of the jaw or infection-induced changes should be taken into account.
2. Potential Diagnoses
-
Bisphosphonate-Related Osteonecrosis of the Jaw (BRONJ):
The patient has a history of long-term intravenous bisphosphonate therapy, and experienced prolonged non-healing of the jaw defect after tooth extraction. Imaging reveals the formation of necrotic bone in the mandible without obvious radiation-related injuries, consistent with the typical clinical features of BRONJ.
-
Osteomyelitis of the Jaw or Infectious Osteonecrosis:
Odontogenic infection or infection after tooth extraction may lead to osteomyelitis of the mandible. However, one should consider whether there are obvious signs of acute or chronic suppuration and systemic inflammatory markers. Given the long-term non-healing condition in this patient, BRONJ should be distinguished from other causes.
-
Bone Metastasis or Tumor Infiltration:
Although the patient has a history of prostate cancer, its bone metastases typically present as osteoblastic (sclerotic) lesions rather than necrotic defects. Nevertheless, it should still be considered in the differential diagnosis and evaluated alongside imaging and clinical features.
3. Final Diagnosis
Based on the patient’s clinical history (prostate cancer, long-term intravenous bisphosphonate use), symptoms (prolonged non-healing of the left mandibular region with pain and swelling following tooth extraction), and imaging findings (localized bone destruction and necrosis of the jaw), the most consistent diagnosis is:
Bisphosphonate-Related Osteonecrosis of the Jaw (BRONJ).
If further confirmation is needed, a biopsy of the local lesion or microbiological culture could be considered to rule out severe infection or other bone pathologies.
4. Treatment Plan and Rehabilitation
4.1 Treatment Strategy Overview
- Infection Control: Based on the clinical situation, consider oral or intravenous antibiotics to control secondary or concurrent infection and select appropriate antimicrobial agents.
- Maintain Oral Hygiene: Avoid further irritation to the local lesion; encourage the use of mouthwash (e.g., 0.12% chlorhexidine) and enhanced oral care to reduce further invasion of necrotic bone and soft tissue by oral flora.
- Discontinue or Assess Bisphosphonate Therapy: Consultation with oncology or endocrinology specialists is recommended to evaluate the risks and benefits of continuing bisphosphonate therapy, and adjust the treatment plan as appropriate.
- Surgical Intervention: For necrotic bone fragments that hinder healing or are associated with uncontrollable infection, surgical debridement and removal of the sequestrum could be considered after infection is strictly controlled. However, the risk-benefit ratio of surgery should be carefully evaluated.
4.2 Rehabilitation and Exercise Prescription
Given the patient is 76 years old with a history of prostate cancer and mandibular disease, rehabilitation should focus on overall health and safety, gradually increasing exercise load.
Below is an example following the FITT-VP principle (Frequency, Intensity, Time, Type, Progression, Volume):
- Frequency: Light to moderate exercise 3–5 times per week.
- Intensity: Start at low to moderate intensity (e.g., walking, basic exercises), and slowly increase based on tolerance.
- Time: 20–30 minutes per session. If the patient has limited endurance, the duration may be split (e.g., 10 minutes × 2–3 sessions).
- Type: Focus primarily on low-impact aerobic activity (walking, stationary cycling) and light resistance training (resistance bands, light dumbbells). Avoid direct impact around the jaw area.
- Progression: Adjust exercise intensity or duration every 2–4 weeks based on tolerance and overall condition, continuously monitoring cardiovascular and musculoskeletal status.
- Volume: Maintain total exercise time per week within a tolerable range (e.g., 60–150 minutes), adjusting according to personal conditions to prevent excessive fatigue or injury.
Important considerations during rehabilitation:
- Avoid strong impact or trauma to the jaw area.
- If pain, swelling, or signs of infection worsen, promptly seek medical advice and adjust exercise intensity.
- Maintain balanced nutrition, and consider calcium, vitamin D, or other essential nutrients as needed to support bone and soft tissue repair.
Disclaimer
This report is a reference analysis based on the available information and cannot replace an in-person consultation or professional medical advice. If you have any questions or if symptoms worsen, please seek medical attention promptly and discuss further treatment options with a specialized physician.
Human Doctor Final Diagnosis
Mandibular Osteonecrosis Associated with Biphosphonate Therapy