


Hemifacial microsomia is a complex syndrome characterized by non-random association of anomalies representing abnormal morphogenesis of first and second pharyngeal arches. Besides facial profile, plain radiographs, cephalometry and Computed Tomography especially volume rendering are used for pre-operative evaluation and post surgical management of patients with craniofacial anomalies.
An 8 year old male child was referred for CT of head and neck for facial asymmetry and hearing difficulties. Clinical examination revealed micrognathia, facial asymmetry and hypoplastic pinna on the right side (Fig 1a). An intraoral examination revealed abnormal dentition, cleft palate with deviated uvula to the right side (Fig 1b). Patient also had right-sided conductive type of hearing loss.
CT head and neck was done using Siemens Somatom 6 slice scanner. High-resolution spiral 3 mm scans were obtained. Additionally 1 mm scans of temporal bone were also obtained. The data was volume rendered and viewed in all planes.
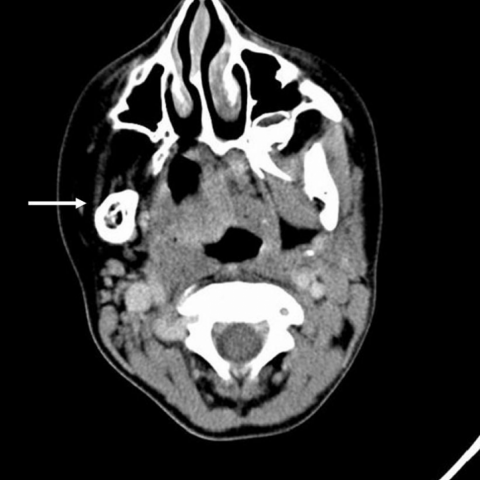
The parotid and submandibular salivary glands were absent on the right side (fig 2a & 2b). The muscles of mastication were also absent or represented by few fibres on the right side (fig 2b).The tongue and uvula were deviated to the same side and palatal defect noted. There was oropharyngeal luminal compromise owing to crowding of soft tissue and bony structures. Incidental tonsilloliths were also seen.
3D reformat and volume rendered images excellently demonstrated hypoplasia of right mandibular ramus along with absence of coronoid process. Additionally, hypoplasia of right maxilla and sphenoid were also noted (Fig 3).
High resolution scans of temporal bone revealed non-development of cartilaginous part of right external acoustic meatus. The bony external canal, mesotympanum and bony ossicles were hypoplastic (Fig 4). The inner ear was unremarkable.
There were no vertebral or ocular or intracranial anomalies noted.
Based on these findings the diagnosis of “Hemifacial Microsomia” was made.
Hemifacial microsomia is one among the large spectrum of oculo-auriculo-vertebral anomalies also referred to as Goldenhar-Gorlin syndrome, first and second branchial arch syndrome or unilateral mandibulofacial dysostosis.
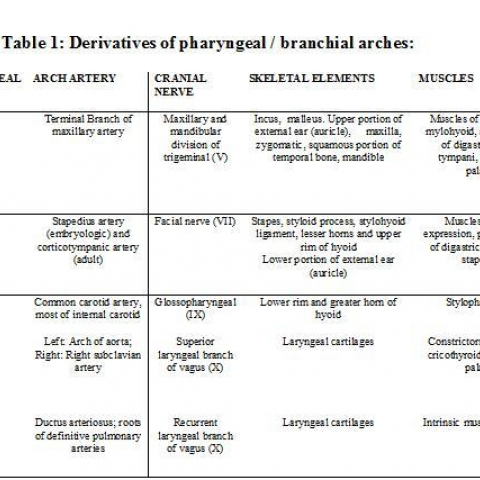
There are five pairs of pharyngeal arches in mammals, numbered 1,2,3,4 and 6 by analogy with their evolutionary origin, the fifth arch having been lost. The first arch is unique in being entirely ectodermal, whereas the others are ectodermal externally and endodermal internally also forming clefts and pouches at their sites of contact respectively. Each arch has its own arch artery and nerve (table 1).
Hemifacial microsomia appears to be directly related to excessive and/or premature cell death in the cell population derived from the first and second ectodermal placodes.
It is either sporadic or autosomal dominantly inherited. There is female preponderance. A widely accepted theory of its pathogenesis centres on abnormal stapedial artery development. Few authors have suggested a possible genetic predisposition to abnormal vascular development, combined with extrinsic factors, leading to bleeding at the anastomosis of the developing stapedial artery. The resulting combination of ischemia and hematoma leads to abnormal formation of the first branchial arch derivatives during weeks 3 through 5 of embryogenesis.
Among the bones, mandible is commonly affected followed by zygoma and maxilla. Anomalies involving mastoid and styloid processes are also seen. In general greatest hypoplasia is seen along the oblique line from the ear to the corner of mouth. Extra skeletal anomalies include hypoplasia of muscles of mastication, malformed or absent auricles, hypoplasia or aplasia of parotid gland. Ectopic salivary glands are often found in such patients. Muscles of mastication show reduced volume proportional to the degree of mandibular hypoplasia.
Hypoplasia of cerebrum, corpus callosum can be associated and usually carry poor prognosis. Ocular findings include dermoid, lipoma or coloboma. Vertebral anomalies can be associated.
Various authors have tried classifying hemifacial microsomia. Pruzansky gave a classification, which graded mandibular deficiency, in 1969. Vento, LaBrie and Mulliken in 1991 gave the OMENS classification. It designates each of the five areas of involvement: 0-orbital, M-mandibular, E-ear, N-facial nerve and S-soft tissue.
The patient was then referred to maxillofacial surgery for distraction lengthening of ramus of mandible. Staged reconstruction of right hearing apparatus was also advised.
The images here vividly describe the syndrome. It also emphasizes the importance of 3D reformatted images, which realistically demonstrate the bony anomalies offering easy guide to the surgeons for treatment planning as well as post surgical management.
Hemifacial Microsomia





Based on the provided clinical images (including lateral facial photographs, intraoral photographs, and cranial CT cross-sectional and 3D reconstruction images), the findings are as follows:
Based on the above imaging findings and the patient's medical history, the main considerations are:
In this case, because the patient demonstrates involvement of tissues derived from the first and second branchial arches (mandibular ramus, external auditory canal, zygomatic bone, masticatory muscle group, etc.) and displays typical unilateral facial underdevelopment, it most closely aligns with the characteristics of hemifacial microsomia.
Combining the patient’s clinical symptoms, imaging evidence, and existing literature, the most likely diagnosis is: Hemifacial Microsomia (Goldenhar-Gorlin Syndrome).
If further evaluation of soft tissue, nerves, and blood vessels is needed, MRI or angiography may be considered. Additionally, interdisciplinary evaluations with ENT, craniofacial surgery, or audiology can help formulate a more comprehensive treatment strategy.
Based on current clinical experience and imaging assessments, the main treatment and rehabilitation recommendations include:
This report provides an academic and reference-based analysis derived from existing clinical and imaging information. It does not replace in-person consultation or professional medical advice. If you have any concerns or if the condition changes, please seek medical attention or consult a specialist for a face-to-face diagnosis and treatment plan.
Hemifacial Microsomia