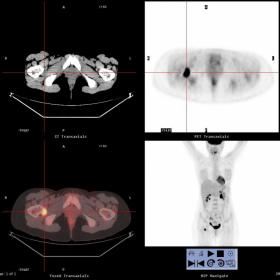


A 41-year-old woman came to our attention because, during a clinical breast examination, a suspicious nodular lesion was found in the left axillary region: the subsequent biopsy revealed metastatic melanoma cells, but the primary lesion was unknown. The patient underwent PET-CT scan for the primary tumour research.
PET-CT showed (Fig. 1) an oval markedly overactive lesion, located between the right small trochanter and femoral external obturator muscle. The woman was therefore sent for MRI in order to further characterize the lesion. MRI showed, in the PET-CT uptake region, a 2.6 x 2.5 cm lesion, without cleavage plane with the external obturator muscle, heterogeneously hypointense on T1-T2 weighted images (Fig. 2, 3, 4)and characterised by intense contrast enhancement (Fig. 5). No significant signal abnormalities compatible with femoral bone erosion were found. MRI could not exclude or confirm the malignant nature of the lesion (secondarism? synovitis nodule? fibromatosis nodule?). CT-guided biopsy was recommended to investigate the nature of the lesion.
Melanoma is a malignant tumour primarily affecting individuals of both sexes between 30 and 60 years. A considerable number of patients presents with clinically evident regional lymph-node metastases and a fair percentage of patients (2%-13%) has occult primary tumour. Survival rates of patients with unknown and with known primary site are similar as well as prognostic factors. PET-CT is the examination of choice to research primary site of malignancy but sometimes it is not conlcusive, thus patients with unknown primary sites of melanoma should be treated as stage III melanomas.
In the presente case, the sole FDG uptake lead to MRI in order to characterize soft tissue lesion. However MRI findings were not univocal since location and morphology was not typical for primary site or eventual metastases and, furthermore, melanin containing lesion may show hyperintensity on T1w sequences for the shortening of T1 relaxation-time.
Second possible diagnosis was a benign lesion such as Pigmented villonodular synovitis (PVNS). PVNS represents an uncommon benign neoplastic process that may involve the synovium of the joint diffusely or focally or that may occur extra-articularly in a bursa or tendon sheath. It should be considered in younger patients (30-40 years) presenting with monoarticular joint symptoms, like limited joint mobility (absent in our case). Pathologic specimens of the hypertrophic synovium may appear villous, nodular or villonodular, and haemosiderin deposition, often prominent, is seen in most cases. PVNS is also referred to as Giant Cell Tumour of the tendon sheath (GCTTS): it has a predilection for lower extremities(knee and hip). Typical MRI findings are a relative low signal mass in T1-T2w sequences, sometimes with scattered areas of hyperintensity: low signal on all pulse sequences (in particular Gradient-Echo sequences) is a typical and nearly pathognomonic characteristic due to haemosiderin presence. After Gadolinium admnistration, PVNS can show intense (like in our case) or moderate enhancement. MRI is optimal for evaluating lesion extent, crucial information to achieve complete surgical resection. PVNS hypervascularity and heterogeneously distributed hypercellularity translate into increased PET-CT uptake.
MRI showed some signal characteristics in disagreement with malignant nature of the lesion, in particular hypo-intensity on T2w images (with and without fat signal suppression) and hypo-intensity on T1w images.
Patient's history of melanoma and PET-CT features raised the doubt of malignancy localization not confirmed at MRI. CT-guided biopsy was requested prior to treatment.
In this presente case, as previously said, patient was treated as stage III melanoma.
Pigmented villonodular synovitis (PVNS) in a patient affected by melanoma





1. On the PET-CT images, a lesion with significantly increased FDG uptake is seen in the left inguinal/hip region (indicated by the arrow), suggesting a metabolically active lesion.
2. MRI sequences show: a localized soft tissue lesion in the same area, with overall low signal on T1-weighted images, and slightly iso- or mildly high signal in some areas; on T2-weighted images (including fat-suppression sequences), the lesion appears predominantly low signal, with possible mild heterogeneous signal in parts of the lesion.
3. The lesion is relatively fixed within the local soft tissue structure, adjacent to the joint capsule or tendon sheath, and demonstrates homogeneous or moderate enhancement, which is consistent with histologically active lesions.
4. The previously diagnosed metastatic melanoma lesion in the left axilla does not show obvious continuous spread to this region on MRI, and no direct link is clearly visible.
5. Overall, the nature of the lesion appears complex, requiring a comprehensive analysis in conjunction with clinical history and pathological findings.
Given the patient’s known history of metastatic melanoma and the current imaging findings, the main considerations include:
1. Metastatic Melanoma:
- The patient has a confirmed diagnosis of metastatic melanoma (axillary metastasis, with the primary site yet to be identified).
- High FDG uptake on PET-CT indicates active metabolism, consistent with a malignant lesion.
- Metastatic melanoma can show variable signal changes, sometimes presenting as high signal on T1 (due to melanin content or hemorrhage), but it can also exhibit complex signal patterns.
2. Pigmented Villonodular Synovitis (PVNS, also known as Tenosynovial Giant Cell Tumor):
- PVNS can also demonstrate significantly increased FDG uptake (suggesting higher metabolic activity), and on MRI, it often appears as low or mixed signal on T1- and T2-weighted images. Low signal on gradient echo sequences is especially common (related to hemosiderin deposition).
- This lesion usually occurs around joints or tendon sheaths, often affecting the lower extremities, with typical symptoms of single-joint pain and restricted movement.
- Although the patient does not present with classic joint symptoms, PVNS remains a differential consideration.
3. Other Soft Tissue Tumors or Focal Lesions:
- Considering the clinical information and imaging findings, other rare soft tissue tumors or even benign lesions cannot be ruled out entirely, though the likelihood is lower.
Taking into account the patient’s confirmed metastatic melanoma in the left axilla, imaging-based assessment of this suspicious lesion in the hip region, as well as subsequent histopathological examination and clinical staging, the most likely diagnosis in this case is: Melanoma (metastatic, Stage III).
If further definitive evaluation is needed, a biopsy or surgical pathology can be performed to confirm. Should pathology reveal a non-malignant lesion, possibilities such as PVNS or other benign processes should be considered.
Treatment Strategy:
1. If, after pathological and staging assessments, the lesion is confirmed to be a Stage III metastatic melanoma, the following treatment options may be considered:
• Surgical Intervention: For resectable local tumors, consider complete surgical resection, possibly with axillary or inguinal lymph node dissection as appropriate.
• Medical Therapy: Includes immunotherapy (such as PD-1 inhibitors) or targeted therapy (such as BRAF/MEK inhibitors).
• Radiation Therapy: Can be chosen for local control or as an adjuvant treatment post-surgery, depending on the situation.
2. If the lesion is ultimately shown to be PVNS or another benign lesion, arthroscopic or open surgical excision of the lesion would be the primary approach, and prognosis is generally more favorable.
Rehabilitation Goal: Under the premise of ensuring effective treatment or surgery, maintain or restore bodily function, improve overall fitness, and prevent muscle atrophy and joint range-of-motion limitations.
Example Exercise Program under the FITT-VP Principle:
1. Frequency: 3–5 times per week.
2. Intensity: Given reduced physical capacity during cancer treatment, begin with moderate to low intensity (e.g., maintaining heart rate at 40%–60% of maximum), increasing gradually.
3. Time: Start with 20–30 minutes per session as an initial target; progress to 40–60 minutes if tolerated.
4. Type: Emphasize low-impact aerobic exercises (e.g., brisk walking, indoor cycling, swimming), supplemented by light resistance training (using resistance bands or light weights).
5. Progression: Reevaluate every 2–4 weeks based on tolerance and overall health, and safely increase exercise intensity or duration in a stepwise fashion.
Individual Precautions:
- In the event of fatigue from surgery, radiation, or chemotherapy, adjust exercise intensity and duration according to daily stamina.
- If local pain, skin breakdown, or other complications occur, stop exercising and seek medical evaluation promptly.
- Monitor cardiac and pulmonary function, especially if there are preexisting cardiovascular or respiratory conditions; conduct a cardiopulmonary assessment before initiating an exercise plan.
Disclaimer:
This report is based solely on the provided medical history and imaging data for preliminary analysis, and should not replace in-person consultation or professional medical advice. Specific treatment plans should be determined according to the actual clinical situation under the guidance of a qualified healthcare professional.
Pigmented villonodular synovitis (PVNS) in a patient affected by melanoma