


A 57-year-old male patient known to have gout presented with an erythematous, swollen and painful left ankle which he described as feeling like an attack of gout. Empirical treatment for 2 months with analgesics and corticosteroids was ineffective. Examination revealed tinea pedis of the left foot and low grade pyrexia.
Ultrasound of the left ankle (Fig. 1) confirmed synovitis, and 1 ml of purulent fluid was aspirated under ultrasound guidance (Fig. 2). Polarised light microscopy of the synovial fluid revealed urate crystals, while culture yielded Staphylococcus aureus. He had an elevated CRP of 244 mg/L (normal range <5), with a normal white cell count of 9.6 x 109/L (normal range 4.0-11.0). Serum uric acid was 345 umol/L (normal range <420).
Radiographs of the left ankle (Fig. 3a) demonstrated joint space narrowing, with erosion of the lateral malleolus which had markedly deteriorated within 3 months (Fig. 3b).
The patient underwent arthroscopy and lavage of the left ankle. He was treated with intravenous flucloxacillin 2g qds for two weeks and then oral flucloxacillin for a further five weeks.
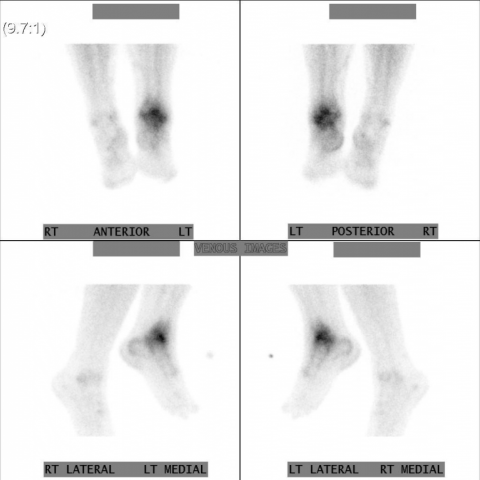
Despite antibiotics symptoms were slow to resolve, and there was considerable residual pain and limitation of movement subsequently, therefore MRI and nuclear imaging were performed (Fig. 4-6).
Gout is caused by deposition of urate crystals in joints, often when serum is saturated with urate (above 420 umol/L). Prevalence is approximately 1%, but varies between populations and is commoner in men [1]. Typical presentation is with a rapid onset of an acute monoarthritis of the great toe, ankle, knee, wrist, finger or elbow, though oligoarticular and polyarticular disease is described, particularly in the elderly. Without specific treatment gout usually resolves within 7-10 days [1]; progressive rather than resolving symptoms and in particular a lack of response to conventional therapies for gout as in the present case should always make one question the diagnosis. The definitive diagnostic test for gout is the identification of urate crystals in synovial fluid; however a normal serum urate level cannot be used to exclude a diagnosis of gout as serum urate levels may fall during an acute attack [1].
Other established rheumatological conditions, including rheumatoid arthritis, can present with an acute monoarticular flare, however the differential diagnoses in the acute situation must include septic arthritis. Importantly, rheumatoid arthritis is recognised as a risk factor for septic arthritis [1-4] particularly if anti-tumour necrosis factor alpha (TNF-alpha) agents are used, which increase the risk of infection at least two-fold [5-7].
Septic arthritis carries a substantial risk of morbidity and mortality. Bacterial septic polyarthritis carries a 30% mortality, while monoarticular disease carries a 4-8% risk [2], with a poor outcome of the infected joint in 45% of the surviving adults [3]. Prompt identification and treatment of septic arthritis can substantially reduce morbidity and mortality. Poor prognostic indicators include older age (>60 years), rheumatoid arthritis, Staphylococcal infection, and a delay in diagnosis.
However, septic arthritis can pose considerable diagnostic difficulty as it does not invariably present with a leucocytosis or pyrexia and the clinical features of gout and septic arthritis can be indistinguishable [8, 9]. Also, the presence of gout crystals in synovial fluid does not rule out septic arthritis [10] and the two conditions may, as in this case, co-exist [8, 11, 12]. The development of septic arthritis in individuals with pre-existing inflammatory joint disease is not uncommon but is frequently associated with diagnostic delay, therefore this case highlights that a high index of suspicion should be cultivated in patients who present with an acutely hot swollen joint [13] and careful consideration should be given to immediate joint aspiration.
Septic bacterial arthritis on a background of gout.








1. X-ray and Ultrasound Findings:
- Marked soft tissue swelling around the left ankle joint, and the joint space may be slightly altered from normal.
- Localized bony changes with irregular margins, suggesting possible chronic inflammation or gout-related bone erosion.
- Doppler ultrasound shows increased blood flow signals around the joint, supporting inflammatory changes.
2. Leukocyte Scintigraphy (Leukoscan):
- Significant leukocyte accumulation in the left ankle joint, indicating active inflammation or infection.
3. MRI Findings:
- Significant synovial thickening and enhancement in the left ankle joint, with exudative effusion in the joint cavity.
- Marked soft tissue edema, suggesting a persistent inflammatory or infectious process.
Synthesizing all imaging data, the left ankle joint displays extensive soft tissue swelling, synovial thickening, and joint effusion. Coupled with findings from functional imaging and the high signal/intense enhancement on MRI, infectious arthritis must be strongly considered.
1. Gouty Arthritis (Acute Gout Flare Alone)
- The patient has a history of gout, which commonly presents as an acute, painful, red, and swollen joint, often affecting the ankle or foot joints.
- However, this episode has persisted for two months without significant relief, and imaging suggests a more extensive inflammatory response, so uncomplicated gout alone may not fully explain the current situation.
2. Gout Complicated by Purulent (Bacterial) Arthritis
- The patient presents with fever (low-grade) and no improvement after standard gout treatments (steroids, pain medications).
- Leukocyte scintigraphy and MRI strongly suggest signs of infection. Gout and infection can coexist. In an acute setting, septic arthritis must be highly suspected.
3. Pure Septic (Bacterial) Arthritis
- If the initial diagnosis of gout was not clearly established, pure septic arthritis could be in the differential diagnosis.
- However, the patient’s known history of gout makes pure septic arthritis relatively less likely, though it must be ruled out.
4. Other Inflammatory Arthritides (e.g., Acute Rheumatoid Arthritis)
- Other inflammatory diseases such as rheumatoid arthritis can present with acute arthritis, but the history is not typical here.
Based on the patient’s known gout history, prolonged persistent joint redness, swelling, and pain, evident inflammatory signs (imaging findings and low-grade fever), and the infectious changes suggested by leukocyte scintigraphy and MRI, the most likely diagnosis is:
“Gout Complicated by Purulent (Septic) Arthritis.”
If culture from joint fluid or blood confirms bacterial involvement, the specific pathogen can be identified. The detection of urate crystals in the joint fluid can further confirm concurrent gout. If diagnostic uncertainty remains, repeated joint fluid analysis and culture are indicated to definitively rule out or confirm bacterial infection.
During the acute phase, appropriate rest and reducing weight-bearing on the affected joint are crucial. After infection control and the acute inflammation subsides, gradual rehabilitation is needed to restore joint mobility and prevent stiffness or muscle atrophy.
Disclaimer: This report is intended for medical reference and discussion only and cannot substitute for in-person clinical diagnosis or the professional judgment of a physician. If there are any concerns or changes in the patient’s condition, please seek medical attention promptly.
Septic bacterial arthritis on a background of gout.