Focal herniation of Hoffa’s fat pad through a retinaculum defect



Clinical History
14 year-old boy with a right knee mass since childhood in the anterolateral aspect of the infra-patellar region, not painful, best visualised during flexion of the knee and disappearing during its extension.
There was no restriction to range of motion and he denied any traumatic event.
Imaging Findings
Ultrasound and MRI images: the patient was in a supine position and a right knee dynamic study (flexion-extension) of the antero-lateral aspect of the infrapatellar region was performed.
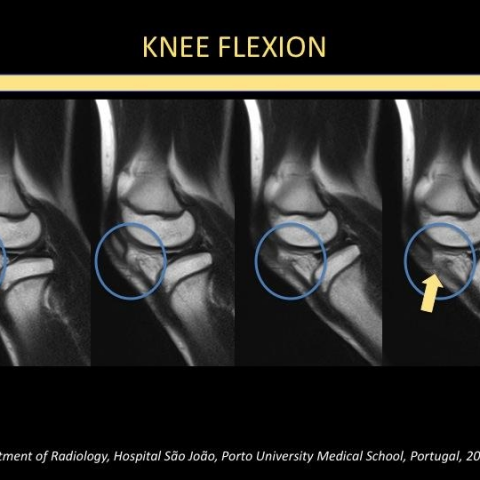
The images demonstrate a focal retinaculum defect that is best visualised during knee flexion (Fig. 1, 4) resulting in herniation of Hoffa's fat pad that is also visualised during knee flexion.
During knee extension the retinaculum fibres get closer to each other, the defect between them becomes smaller and Hoffa's fat pad herniation is not so clearly depicted (Fig. 2, 5).
The MR images (Fig. 4,5) show with more detail the soft tissue components of the knee and also reveal the more pronounced retinaculum defect during knee flexion. There is no bone marrow edema suggesting the absence of recent traumatic event.
Figure 3 is a parasagittal T1 weighted MR image that reveals the anatomy of the surrounding structures.
Discussion
Anterolateral stabilisation of the knee is provided by the capsule (capsular ligament) and iliotibial tract. The anterior part of the capsule is reinforced by the superior and inferior retinacula and the vastus lateralis muscle [1].
The lateral retinaculum appears as a hyperechoic band originating from the iliotibial band and the vastus lateralis muscle. It runs obliquely and transversely and inserts on the patella and the patellar tendon, and is composed of two layers.
A tear of the retinaculum is mostly seen after dislocation of the patella. The retinaculum may either tear completely or partially. A history of direct trauma resulting in a focal retinaculum defect or simple inspection of the skin for surgical scaring will determine the cause of the lesion. If the repair of the retinaculum is insufficient, herniation of Hoffa's fat pad can occur and is best visualised and accentuated during flexion of the knee. The fat pad should be clearly seen as a heterogeneous hypoechoic mass bulging through the retinaculum. In acute impingement of fat, the overlying subcutaneous fat becomes hyperechoic, consistent of inflammatory changes. Rarely, direct impact can lead to a focal defect in a retinaculum [2].
Although in our case no history of trauma or previous surgery was mentioned, probably this focal retinaculum defect was originated by an old traumatic event that the patient did not remember. Our patient did not mention any pain either, probably because there is no impingement of fat nor vascular restriction.
Although the current literature rarely mentions the herniation of Hoffa's fat pat associated with retinaculum defect, we believe that this kind of presentation with a bulging mass overlying the retinaculum that becomes more conspicuous during knee flexion is very suggestive of this pathology.
Careful anamnesis of the patient (medical history of previous traumatic episode or surgery) may already suggest the correct diagnosis [2].
Magnetic Resonance provides high resolution images for the different soft tissues of the knee, and in cases of recent trauma can depict bone marrow edema however, due to its dynamic capabilities, ultrasound is the imaging modality of choice to confirm this diagnosis. Furthermore, ultrasound is more widely available, faster and less expensive.
Differential Diagnosis List
Final Diagnosis
Retinaculum partial defect/rupture with herniation of Hoffa's fat pad
Liscense
Figures
Knee flexion - Parasagittal T1 weighted MRI.
Knee extension - Parasagittal T1 weighted MRI.

Knee extension - Ultrasound

Knee flexion - Ultrasound

Knee anatomy - Parasagittal T1 weighted MRI.

1. Imaging Findings
Based on the provided imaging (including knee flexion and extension MRI and ultrasound images) and the patient’s medical history, the following observations have been made:
- A localized soft tissue protrusion is observed beneath the patella on the right knee, in the area of the lateral retinaculum (lateral supporting structure). The protrusion becomes more pronounced during knee flexion and disappears or diminishes with knee extension.
- Ultrasound indicates an interruption in the continuity of the lateral retinaculum fibers, forming a localized defect; with the knee flexed, the Hoffa’s fat pad (infrapatellar fat pad) appears to protrude or “herniate” into this defect.
- No significant inflammatory changes or signs of vascular compression are noted in the surrounding soft tissues. There is also no evidence of bone destruction or fracture.
2. Potential Diagnoses
Based on the imaging features above and the patient’s history, the following potential diagnoses and considerations are proposed:
-
Localized Defect of the Lateral Retinaculum with Hoffa’s Fat Pad Herniation
— Characteristics: The integrity of the lateral retinaculum is disrupted, creating a localized defect through which the fat pad may protrude during knee movement (particularly flexion). The absence of significant pain suggests no prominent inflammation or mechanical impingement. -
Partial Tear of the Lateral Retinaculum with Poor Healing
— Characteristics: A history of minor trauma or surgery (possibly forgotten or unnoticed by the patient) could lead to a disruption of the fibers, forming a defect. Imaging findings may resemble fat pad herniation. -
Other Less Common Soft Tissue Lesions (e.g., Synovial Cyst, Fibroma, etc.)
— Characteristics: Various neoplastic or cystic changes may present as localized swelling. However, they typically show less dynamic change with knee flexion/extension, and ultrasound/MRI findings usually differ from those of fat pad herniation.
3. Final Diagnosis
Considering the patient’s age, symptoms, medical history (even though the patient denies any trauma, minor or forgotten trauma cannot be ruled out), and the dynamic imaging findings on both ultrasound and MRI, the most likely diagnosis is:
Lateral Retinaculum Defect with Hoffa’s Fat Pad Herniation (a localized structural change without significant clinical symptoms)
4. Treatment Plan and Rehabilitation Program
Since the patient currently has no significant pain or functional limitations, and there are no signs of active inflammation, a conservative or observational approach is generally recommended:
- Conservative Treatment
- If there is no pain, discomfort, or functional impairment, observation with regular follow-ups is advised.
- During daily activities, avoid high-intensity or excessive knee flexion/extension that could cause secondary injury.
- Use of a knee brace or elastic bandage may provide moderate lateral support.
- Surgical Treatment
- Surgical repair of the defect in the lateral retinaculum should be considered only if persistent pain, mechanical catching/locking, or limited joint function occurs.
- The surgical goal is to restore fiber continuity and address any potential fat pad impingement.
Rehabilitation and Exercise Prescription Recommendations (FITT-VP Principle)
- Frequency
- Perform knee function training at low to moderate intensity 3–4 times per week.
- Intensity
- Begin with light resistance exercises while closely monitoring knee response.
- If no discomfort arises, consider gradually increasing resistance or difficulty after 2–3 weeks.
- Time
- Each training session should last 20–30 minutes, with possible gradual extension based on tolerance.
- Type
- Early-stage exercises may include wall-sits, seated straight leg raises, or knee flexion/extension with resistance bands.
- If pain-free, consider progressing to closed-chain lower limb strengthening, such as light-weight partial squats.
- Volume & Progression
- Gradually increase difficulty based on joint stability and pain, for example by using stronger resistance bands or adding small weights.
- Avoid sudden, large increases in training volume or load to prevent soft tissue irritation.
Throughout the rehabilitation process, closely monitor for knee swelling, pain, or restricted range of motion. If any abnormality occurs, stop training immediately and consult a specialist.
Disclaimer: This report is for reference only and does not replace in-person consultations or professional medical advice. If you have any concerns or if symptoms worsen, please visit a hospital or consult an orthopedic/sports medicine specialist promptly.
Human Doctor Final Diagnosis
Retinaculum partial defect/rupture with herniation of Hoffa's fat pad