Scaphotrapeziotrapezoidal (STT) osteoarthritis



Clinical History
A 53-year-old male military officer presented with complaints of chronic localised pain on the thumb basilar area of his dominant hand along with decreased grip strength. Medical history revealed a hand injury 2 years before in a motor vehicle accident that was treated with simple splinting. No fracture was reported.
Imaging Findings
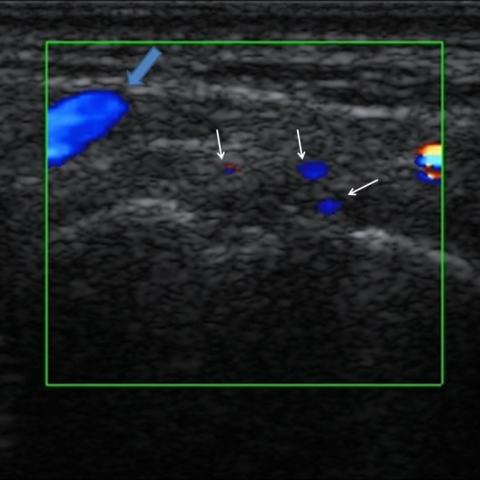
The mechanism of his initial hand trauma was described as a high energy force applied axially on his outstretched palm (the patient was injured with his steering wheel during the collision). Mild swelling and tenderness on palpation over the thenar eminence was noticed on physical examination. Plain radiographs showed sclerosis of the scaphoid-trapezium-trapezoid articulating surfaces with associated joint space narrowing (Fig. 1). An ultrasound examination was performed subsequently that demonstrated irregularity of the scaphotrapezoidal articulation along with findings of accompanying synovitis (Fig.2). An MRI examination verified the aforementioned findings and relying on the clinical and imaging features, the clinicians suggested an MDCT examination in order to better delineate the joint pathology and the associated osseous surfaces (Fig. 3-4). The patient’s clinical history, together with the imaging findings established the diagnosis of a scaphotrapeziotrapezoidal (STT) posttraumatic osteoarthritis (Fig. 5) and the patient was referred to a specialised hand surgery clinic for possible surgical treatment.
Discussion
The clinical evaluation and treatment of chronic wrist pain can often be a challenging diagnostic dilemma because the aetiology is broad and includes both intracarpal and intercarpal pathology [1-2]. With recent improvements in diagnosis and imaging of carpal disorders, the radiologists are able to confirm a clinical suspicion of injury and thus tailoring the appropriate therapy [1-3]. Scaphotrapeziotrapezoidal (STT) joint osteoarthritis has been estimated to account for 13% of all wrist arthritis cases and can cause significant pain and limitation of function [4-6]. Common predisposing factors are trauma, an abnormal trapezio-trapezoidal inclination and laxity of the capitotrapezial ligament [4-6]. Although the underlying pathophysiologic mechanisms that may lead to posttraumatic osteoarthritis are not well understood and clarified, studies have shown that the degree and severity of articular cartilage damage and the joint surface incongruity both correlate with the development of osteoarthritis [7]. STT arthritis is usually manifested with pain, swelling and stiffness over the thumb base and physical examination might reveal local tenderness and a radial grind in chronic cases [4-6]. However the clinical signs and symptoms are not considered pathognomonic and differential diagnosis from other causes such as scaphoid disorders, trapezio-metacapal osteoarthritis, DeQuervain tenosynovitis, symptomatic ganglion cysts may be required [4-6]. Therefore the radiologic evaluation is of paramount importance in treatment planning. Plain radiographs may be normal early in the setting of STT arthritis, while in advanced stages show the characteristic osteoarthritic features. High resolution ultrasonography of the small joints may provide additional information by revealing the accompanying synovial reaction and inflammation [8]. MRI has become an important diagnostic tool for evaluation of chronic hand and wrist pain because it can identify both intracarpal and intercarpal abnormalities [1-3]. In our case MRI verified the radiographic and ultrasonographic findings and also showed bone marrow oedema in the articulating bones of the STT joint. Furthermore an osteochondral defect was identified in the capitate bone, which was attributed either due to STT osteoarthritis and altered local biomechanics or as a result of the remote trauma. MDCT with its superior spatial resolution together with the availability of multiplanar reformations can delineate the osteoarthritic changes equally or even better than plain MRI [9]. STT arthritis is initially treated conservatively with splinting, oral analgesics or local corticosteroid injections. In advanced cases surgical treatment consists primarily of fusion of the STT joint, but alternative operative techniques include trapeziectomy, excisional arthroplasty, and prosthetic replacements [4-6, 10].
Differential Diagnosis List
Final Diagnosis
Scaphotrapeziotrapezoidal (STT) osteoarthritis
Liscense
Figures
Radiograph

Ultrasonographic examination

MRI examination



MDCT examination





Correlation of imaging findings

Medical Imaging Analysis Report
I. Imaging Findings
Based on the provided X-ray, ultrasound, MRI, and MDCT images, the main imaging features include:
- In the radial wrist area, especially involving the scaphoid, capitate, trapezium, trapezoid, and their related joint surfaces, notable bony sclerosis, joint space narrowing, and marginal osteophyte formation are observed, suggesting degenerative changes.
- MRI shows bone marrow edema below the joint surfaces (high signal on T2-weighted or STIR images), indicating local bone reaction and inflammation; a possible mild subchondral bone defect (osteochondral lesion) is noted in the capitate.
- Ultrasound reveals local soft tissue thickening, synovial reaction, and increased perijoint blood flow signals, suggesting chronic inflammation and synovial hyperplasia.
- With its higher spatial resolution, MDCT further demonstrates bony overgrowth and irregular joint surfaces of the STT (scaphotrapeziotrapezoid) joint, enhancing the assessment of skeletal structural changes.
II. Potential Diagnoses
Taking into consideration the patient’s history (wrist trauma two years ago, chronic radial wrist pain, and decreased grip strength) and the above imaging findings, the following should be considered as possible diagnoses or differential diagnoses:
- Post-traumatic Scaphotrapeziotrapezoid (STT) Joint Arthropathy
- The previous history of trauma, clinical presentation of radial wrist pain, and weakened grip strength, along with imaging findings of articular degeneration, osteophyte formation, and bone marrow edema, are consistent with post-traumatic arthritis.
- Trapeziometacarpal (TMC) Osteoarthritis
- Commonly seen in thumb base pain; however, in this case, the primary lesions are focused on the STT joint, so TMC osteoarthritis is mainly considered as a differential diagnosis.
- Other Scaphoid Lesions (Fracture, Avascular Necrosis)
- Although there is a history of old trauma, there are no classic signs of scaphoid nonunion or avascular necrosis, so these can be preliminarily ruled out.
- Radial-sided Tenosynovitis (e.g., De Quervain’s Tenosynovitis)
- Typically presents with pain over the first dorsal compartment (abductor pollicis longus and extensor pollicis brevis), often activity-related. However, no obvious tendon sheath swelling or abnormal thickening was seen on imaging.
- Radial Ganglion Cyst
- While a cystic mass may form on the radial side of the wrist, no typical cystic structure or definitive fluid signal was noted on imaging.
III. Final Diagnosis
Considering the patient’s age, symptoms (radial wrist pain, decreased grip strength), history of trauma (treated after a car accident), and imaging findings (significant degenerative changes at the STT joint surfaces, bone marrow edema, osteochondral involvement), the most likely diagnosis is:
Scaphotrapeziotrapezoid (STT) Joint Osteoarthritis (Post-traumatic Degenerative Changes).
If needed, further evaluation with arthroscopy or follow-up imaging during clinical treatment could help clarify the extent of cartilage damage and joint stability.
IV. Treatment Plan and Rehabilitation
1. Conservative Treatment
- Rest and Splinting: During acute or flare-up phases of chronic pain, use a wrist or thumb spica splint to reduce joint loading and range of motion, thereby alleviating symptoms.
- Medications and Physical Therapy: Oral or local injection of nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and inflammation. Physical therapy (e.g., ultrasound therapy or heat therapy) can improve local circulation and relieve discomfort.
- Rehabilitation Exercises: Once pain subsides, initiate gentle range-of-motion exercises and muscle-strengthening programs, avoiding excessive force or sudden twisting motions.
2. Surgical Treatment
- Indications for Surgery: If the disease progresses to a late stage or conservative treatment fails, surgical options such as STT joint fusion, arthroplasty, partial or complete bone resection (e.g., excision of the trapezoid alone or total joint replacement) may be considered.
- Postoperative Rehabilitation: Usually involves weeks to months of splinting, followed by guided functional training to prevent joint stiffness and restore grip strength.
3. Rehabilitation/Exercise Prescription Recommendations (FITT-VP Principle)
- Frequency (F): 3-4 sessions per week of specialized rehabilitation exercises for the wrist and thumb.
- Intensity (I): Focus on light-to-moderate resistance, avoiding vigorous or pain-threshold-exceeding exercises. Initially, use resistance bands or soft grip balls.
- Time (T): 10-15 minutes per session, gradually increasing duration according to tolerance.
-
Type (T):
- Wrist and thumb range-of-motion exercises: gentle flexion-extension, abduction, and circumduction movements.
- Muscle strengthening: use a tennis ball or grip ball to perform gentle squeeze-relax drills, gradually increasing resistance.
- Proprioception training: fine motor tasks like threading beads or pinching small objects to enhance hand dexterity.
- Progression (P): As pain improves and range of motion increases, resistance and complexity can be gradually increased. If severe discomfort or recurring pain occurs, reduce intensity or pause the exercises.
- Volume (V) & Individualization (P): Adjust the duration and content of each session according to the patient’s condition and subjective perception. Tailor the program around the individual’s daily activities and occupational demands.
Special Note: If the patient has osteoporosis or other joint disorders, exercises should be guided by a physician and rehabilitation therapist to progress gradually, with caution to prevent falls or further injury.
Disclaimer
This report is a reference medical analysis based on available data and cannot replace professional, in-person medical diagnosis and treatment. If you have any questions or changes in your condition, please seek medical attention or consult a specialist promptly.
Human Doctor Final Diagnosis
Scaphotrapeziotrapezoidal (STT) osteoarthritis