An unusual case of metatarsalgia



Clinical History
This 42-year-old female patient was admitted to our institution reporting pain and swelling on the ball of her left foot, especially localised at the metatarsophalangeal joint of the second toe. The patient was a flight-assistant and she reported repetitive use of high-heels shoes. MR and US evaluation were performed.
Imaging Findings
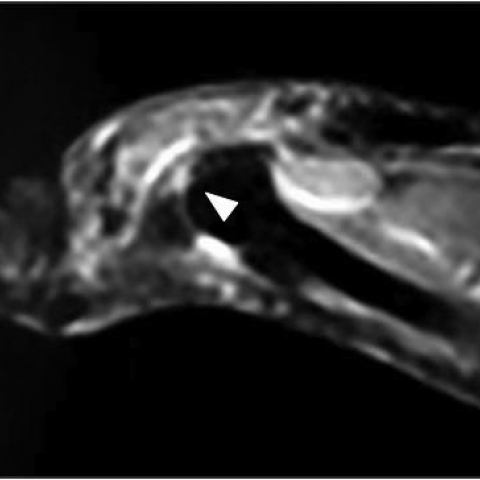
MR examination of the left foot, performed with a low-field (0.18T) extremity-dedicated MRI system, revealed oedematous thickness of soft tissues surrounding the second toe metatarsophalangeal (MTP) joint, with signal alteration on the plantar side, in keeping with plantar plate tear (Fig. 1). An ultrasound examination was performed to better investigate the MTP joint: US evaluation showed a hypo-echoic defect on the lateral side of the plantar plate, confirming the presence of a partial tear in the distal part of the plantar plate (Fig. 2).
Discussion
The plantar plate is a fibrocartilaginous structure localised near the metatarsophalangeal (MTP) joint; it has a proximal attachment to the periosteum of the metatarsal diaphysis and a distal insertion directly to the plantar side of the proximal phalanx. The plantar plate has a central position and presents multiple important attachments to the collateral ligaments, to the plantar fascia, to the inter-metatarsal ligaments and to the fibrous sheath of the flexor tendons: as a consequence, it is easy to understand the important bio-mechanical role of the plantar plate as a central stabiliser of the metatarsophalangeal joint. Static stabilisation of the MTP joint is primarily function of the plantar plate, while dynamic stabilisation is provided by the extrinsic and intrinsic muscles of the forefoot, and their ability to stabilise the joint depends on the integrity of the plantar plate. After rupture of the plantar plate, the proximal phalanx tends to subluxate dorsally, and the extensor tendons are unable to extend the interphalangeal joints. MTP joint instability presents clinically with pain in the forefoot; symptoms may include swelling, malalignment, neuritic symptoms and dysfunction in the normal articular bio-mechanics of the foot. MTP joint instability can be associated with extra- and intra-articular conditions, and the differential diagnosis comprehends pathologies such as Morton's neuroma, synovial cysts or Freiberg’s infraction [1].
At MR imaging, features of plantar plate rupture correspond to substitution of the normal hypo-intense area with a focal hyper-intense finding. Sagittal images can provide a better evaluation of the thickness of the tear, while coronal images allow establishing the position of the lesion [2]. It is important to underline that only high-field MR can provide a diagnosis and it should be considered the gold standard in evaluation of plantar plate ruptures; however, in selected cases, US examination can add insightful information to achieve a complete understanding of the MTP joint condition. At US rupture of plantar plate presents as a loss of the normal homogeneous structure and tears appear as little hypoechoic defects in the context of distal insertional fibers: tears could occur as partial-thickness lacerations or as full-thickness lacerations. Most of the tears occur at the distal attachment on the proximal phalanx [3].
In conclusion, a correct clinical approach and a diagnostic iter in which dynamic US can play a considerable role are fundamental to achieve a correct diagnosis of metatarsophalangeal joint instability, a condition often unrecognised and potential source of frustration for the orthopaedic surgeon.
Differential Diagnosis List
Final Diagnosis
Plantar plate partial-thickness tear
Liscense
Figures
MR examination

US examination


1. Imaging Findings
This patient is a 42-year-old female presenting with pain and local swelling in the plantar forefoot area of the left foot (primarily at the second metatarsophalangeal joint). Based on the provided MRI and ultrasound images, the following key features are noted:
- MRI Imaging: Near the plantar side of the second metatarsophalangeal joint adjacent to the plantar plate, the originally low-signal fibrocartilaginous structure is replaced by a localized high-signal lesion, suggesting possible disruption of the fibrous continuity. Sagittal sequences help assess tear thickness, while coronal sequences are more useful for localizing the tear.
- Ultrasound Imaging: The normally homogeneous plantar plate structure shows a focal hypo-echoic (low echo) defect at the distal attachment, indicating a possible partial or full-thickness fiber tear. This commonly occurs near the attachment site on the proximal phalanx, consistent with typical plantar plate tear locations.
- Local Soft Tissue Condition: Mild soft tissue swelling is visible around the joint, and the joint capsule and supporting ligaments may be strained or exhibit inflammatory changes.
2. Potential Diagnoses
Based on the patient’s frequent use of high heels, the forefoot (metatarsal head) pain, and the imaging findings indicating joint instability and plantar plate fiber damage, the possible diagnoses include:
- Partial or Full-Thickness Tear of the Plantar Plate: The plantar plate is located under the metatarsophalangeal joint and is crucial for joint stability. Frequent high heel wear leads to excessive pressure on the forefoot and repetitive microtrauma. A tear would appear as a localized high signal on MRI and a hypo-echoic defect on ultrasound, consistent with the clinical and imaging findings.
- Morton’s Neuroma: Usually presents with intermetatarsal pain, commonly affecting the 3rd and 4th interspaces but can sometimes involve the 2nd and 3rd. MRI or ultrasound may show localized thickening of the intermetatarsal nerve sheath. Patients often report numbness or burning pain, and pain can be elicited by squeezing the foot, which is less typical for this case.
- Freiberg’s Infraction (Freiberg Disease): Commonly involves osteonecrosis of the second or third metatarsal head. MRI may show bone marrow edema or collapse of trabeculae. Patients often experience pain in the metatarsal head that worsens with activity, and imaging typically reveals bony changes. This case does not clearly indicate bone collapse or necrosis.
- Joint Capsule or Synovial Cyst: A cystic mass can be found around the joint; ultrasound may show anechoic or hypo-echoic areas, and MRI may show a cystic signal. However, the main abnormality here is focused on the course of the plantar plate fibers, making an isolated cystic lesion less likely.
3. Final Diagnosis
Taking into account the patient’s age, occupational factors (prolonged high heel use resulting in increased forefoot pressure), clinical symptoms (pain and instability at the second metatarsophalangeal joint), and imaging findings (MRI and ultrasound indicating disruption and hypo-echoic defects in the plantar plate fibers), the most likely diagnosis is:
A partial or full-thickness tear of the plantar plate at the second toe (Plantar Plate Tear).
4. Treatment Plan and Rehabilitation
4.1 Treatment Overview
- Conservative Treatment:
- Reduce factors that cause excessive load on the plantar plate, such as avoiding prolonged use of high heels and opting for wider footwear with arch support.
- Use protective insoles or orthotic devices to relieve local pressure on the forefoot and prevent further plantar plate damage.
- Apply local anti-inflammatory and analgesic treatments or use physical modalities (e.g., ultrasound therapy, ice packs, iontophoresis) to reduce inflammation and pain.
- Surgical Treatment:
- Indicated if conservative management fails, or if there is significant joint instability or deformity of the metatarsophalangeal joint. Surgical repair of the plantar plate combined with soft tissue stabilization may be considered.
4.2 Rehabilitation and Exercise Prescription
Rehabilitation should follow a gradual, individualized approach, guided by the FITT-VP principle:
- Type of Exercise: Begin with non-weight-bearing or low-impact activities such as swimming, passive joint mobilization in a seated position, or resistance band exercises. Progress to light weight-bearing walking in the intermediate phase, and eventually resume daily walking and light jogging if tolerated in the final phase.
- Frequency: It is recommended to perform low-intensity exercises 3–5 times per week initially, increasing to short daily sessions as tolerated and based on pain and recovery.
- Intensity: Start at a low intensity to avoid repeated stress that can cause re-injury. Increase resistance or load gradually, following pain feedback and medical advice.
- Time: Begin with 10–20 minutes per session, increasing to around 30 minutes as tolerated.
- Progression: Transition from low-intensity to moderate-intensity exercise, maintaining protective support for the affected joint (such as arch supports or bracing). If significant pain or swelling occurs, reduce the exercise intensity immediately and seek further evaluation.
Special Considerations: For patients with particularly fragile feet or marked forefoot pain, it is important to evaluate lower limb alignment and arch integrity. Those with cardiac or pulmonary issues or other comorbidities should consult healthcare professionals for a more cautious exercise plan.
Disclaimer: This report is a reference analysis based on the provided information and does not replace an in-person medical consultation or professional medical opinion. For any concerns or changes in condition, please seek prompt medical attention or consult a specialist.
Human Doctor Final Diagnosis
Plantar plate partial-thickness tear