Solitary Bone Cyst



Clinical History
A 10-year-old boy presents to the Emergency Department with acute and spontaneous pain in the left hip, after playing a football-game.
At clinical examination, there was focal tenderness around the greater trochanter and pain at flexion and rotation of the hip.
Imaging Findings
On conventional radiographs of the hip, a well-circumscribed, radiolucent lesion was seen in the central metaphysis of the femur, without periosteal reaction. The lesion appeared multilocular and was described as "soap-bubble"-like.
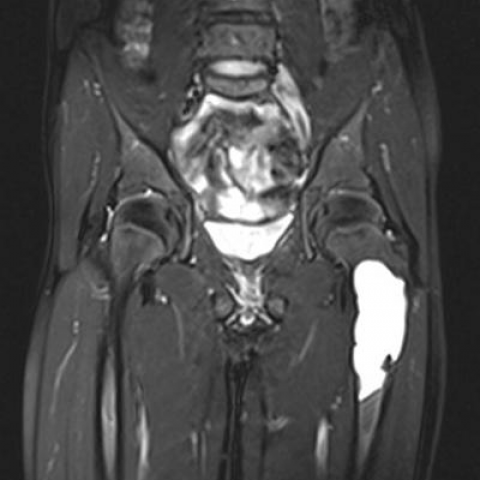
Subsequent magnetic resonance imaging (MRI), revealed the lesion to be of high signal intensity on fat suppressed T2-weighted images (WI) and isointense to muscle on T1-WI.
After intravenous administration of gadolinium, peripheral rim-enhancement was seen, whereas the central part of the lesion was not enhancing. Sagittal images showed no fluid/fluid levels.
Based on these findings, the diagnosis of a Solitary Bone Cyst was made.
Because no pathologic fracture was seen, the patient’s pain was attributed to muscle contusion and the patient was initially treated with pain relievers and relative rest.
Because of the increased fracture risk due to the cortical thinning, a dynamic hip screw was placed.
Discussion
Solitary bone cysts (SBC) are defined as "tumour-like lesions of unknown etiology, attributed to local disturbance of bone growth" [1].
Because SBC’s occur in patients whose growth plates are not yet or recently closed, patients are young (85% <20 years old) [2].
The lesions are usually located in the central metaphysis of long bones, most often the proximal humerus or femur, although a wide variety of locations has been described. Involvement of the calcaneus and/or ilium occurs in adult patients [1, 3].
Uncomplicated SBC's are merely asymptomatic, but occasionally, pain or stiffness may be present in the adjacent joint.
Large lesions are at risk for pathologic fracture through the cyst, and some patients present with acute pain following these fractures [1].
On conventional radiographs, SBC's present as well-circumscribed, radiolucent lesions in the central metaphysis. Their long axis parallels the long axis of the affected bone.
They can appear multilocular on plain films, due to projection of the ridging of the walls of the cyst (pseudotrabeculation) but are macroscopically always unicameral.
After a pathologic fracture, small bony fragments may migrate through the fluid-filled cavity and create a pathognomonic 'fallen fragment sign': a fragment of cortical bone attached to the periosteum or lying in the dependent part of the lesion [3-5].
On MR-imaging, SBC's show the typical features of cysts, i.e. high signal intensity on T2-WI and low on T1-WI. After intravenous gadolinium-administration , a thin rim of peripheral enhancement is seen [5].
When a fracture has occurred, signal intensity on T2-WI may become heterogeneous, due to intralesional bleeding.
The most important differential diagnoses are [1]:
- Aneurysmal bone cysts: more eccentric located, fluid/fluid-levels on T2-WI.
- Fibrous dysplasia: ‘ground glass’ appearance on radiographs, variable appearance on MR-imaging (MRI does not provide additional information).
- Brodie abscess: causes severe pain, surrounding bone marrow oedema on MRI.
- Giant cell tumours: adult patients, juxta-articular location, heterogeneous intensity on T2- and T1+Gd –WI.
Asymptomatic SBC’s require no treatment and regress spontaneously after closing of the growth plates.
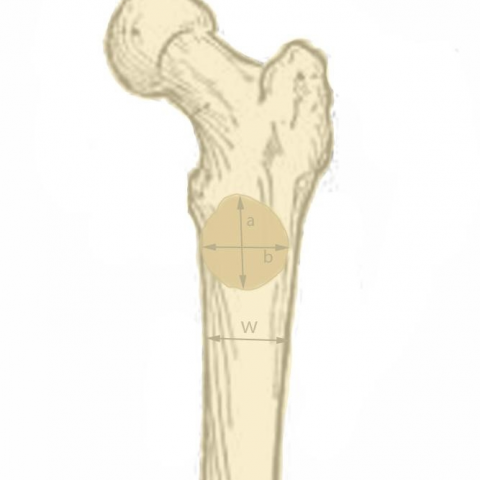
Occasionally, treatment is advocated due to risk of pathologic fracture. The most accurate predictor of fractures is the Bone Cyst Index (BCI). SBC's with BCI larger than 3.5 (femur) or 4 (humerus) are at risk for pathologic fracture. Size of the lesion and cortical thinning are poorly correlated with fracture-risk. [6]
Possible treatments include curettage, corticoid injection, bone grafting or DHS placement (proximal femur).
Cysts that are complicated by a pathologic fracture usually regress during healing of the fracture.
Differential Diagnosis List
Final Diagnosis
Solitary/Unicameral/Juvenile Bone Cyst (SBC)
Liscense
Figures
Conventional radiography

Coronal MR-images before intravenous gadolinium administration

Axial T1-WI after intravenous gadolinium administration

Post-operative radiograph

Bone Cyst Index
Medical Imaging Analysis Report
I. Imaging Findings
The patient is a 10-year-old boy who developed acute, spontaneous pain in the left hip region after physical activity. Based on the provided imaging data (including X-ray and MRI), a notable cystic lesion is observed in the left proximal femur (near the trochanteric region):
- On X-ray: There is a lucent area in the central region of the proximal femur with clear definition and relatively regular boundaries. The cortical bone appears thinned but does not show obvious invasion of the surrounding tissues. The lesion shows a single-chamber feature, and slight cortical expansion can be observed corresponding to the cystic area.
- On MRI: The lesion demonstrates low signal on T1-weighted images and high signal on T2-weighted images, consistent with a cystic characteristic. After contrast enhancement, a thin rim enhancement is observed, aligning with common enhancement patterns in cystic bone lesions.
- Clinical examination shows local tenderness and pain with joint movement, suggesting a possible pathologic fracture or impending fracture. If a “Fallen Fragment Sign” is present, it would further suggest an internal fracture fragment within the cystic lesion.
II. Potential Diagnoses
Based on the patient’s age, imaging findings, and clinical presentation, the following diagnoses or differential diagnoses are considered:
- Solitary Bone Cyst (SBC): Commonly seen in children and adolescents, often located in the metaphysis of long bones. X-ray demonstrates a well-defined radiolucent area, MRI shows a cystic lesion, and post-contrast imaging often reveals a thin rim enhancement.
- Aneurysmal Bone Cyst (ABC): Often presents as an eccentric destructive lesion. On MRI, multiple septations and typical fluid-fluid levels may be visible. This case does not show the characteristic fluid-fluid levels on imaging.
- Fibrous Dysplasia: On X-ray, a “ground-glass” appearance is commonly observed. However, this case shows a well-defined lucent area with a distinct cystic characteristic, which does not match fibrous dysplasia.
- Brodie’s Abscess: Typically accompanied by a sclerotic margin, significant pain, and prominent bone marrow edema, often associated with a chronic or subacute infection. There are no obvious signs of infection in this case.
- Giant Cell Tumor (GCT): More frequently seen in adults (after epiphyseal closure) and usually located near joints. On MRI, GCTs often exhibit a heterogeneous signal. Given this patient’s young age and the lesion’s morphology, a benign cystic lesion is more likely.
III. Final Diagnosis
Considering the patient’s age, pain characteristics, and imaging findings (a single-chamber cystic radiolucent area, thin rim enhancement, located in the proximal femur near the trochanteric region), the most likely diagnosis is a Solitary Bone Cyst (SBC).
If subsequent imaging follow-up or pathological examination confirms these features, the diagnosis can be definitively established.
IV. Treatment Plan and Rehabilitation
(A) Treatment Strategy
- If the lesion is small and shows no significant clinical symptoms, conservative observation may be considered. Regular imaging follow-up is recommended since solitary bone cysts often tend to improve or significantly decrease in size after physeal closure.
-
If the lesion is large with a clear risk of pathologic fracture, the following interventions may be considered:
- Corticosteroid Injection: May facilitate closure or shrinkage of the cyst.
- Curettage and Bone Grafting: Indicated for larger lesions or those with a pathologic fracture.
- Internal Fixation: For lesions in the proximal femur that have fractures or a high risk of fracture, dynamic hip screw (DHS) or other fixation methods may be employed to maintain stability and promote healing.
(B) Rehabilitation / Exercise Prescription
A gradual rehabilitation program based on the FITT-VP principle is recommended, tailored to the type of surgery or conservative treatment:
-
Early Phase (Postoperative or early conservative treatment):
- Frequency: Several sessions of light activity per day, such as bed-based or seated joint mobility exercises.
- Intensity: Low-intensity; avoid excessive weight-bearing and overly large ranges of motion of the hip joint.
- Time: 5–10 minutes per session, repeated multiple times per day.
- Type: Primarily non-weight-bearing active joint exercises, isometric quadriceps contractions, etc.
- Progression: Gradually increase the range of motion and duration according to pain tolerance and healing progress.
-
Mid-Phase Rehabilitation (around 6–8 weeks after fracture or surgery, depending on bone healing):
- Frequency: 3–5 times per week.
- Intensity: Moderate intensity; gradually allow partial weight-bearing, such as standing and walking training with the assistance of crutches.
- Time: 15–20 minutes per session, progressively increasing to about 30 minutes.
- Type: May include aquatic exercises, stationary cycling, and core stability training to reduce direct impact on the hip.
- Progression: Gradual increase in weight-bearing with protective bracing, progressing to standing balance training.
-
Late-Phase Rehabilitation (12 weeks or more after fracture or surgery):
- Frequency: 3–5 times per week, maintaining moderate intensity.
- Intensity: Progressively return to near-normal activity levels; under professional guidance, light jogging or strength training may be introduced if appropriate.
- Time: At least 30 minutes per session, alongside daily activities.
- Type: Incorporate functional training such as balance exercises, low-impact plyometric drills, and hip and lower-limb strengthening.
- Progression: Aim for a gradual return to athletic activities. If necessary, reduce high-impact activities and continue imaging follow-up.
Throughout the rehabilitation process, special attention should be paid to the growth characteristics of the child’s bones and overall bone health. Avoid strong impacts or excessive weight-bearing that may increase the risk of recurrent fractures. Regular imaging follow-up is recommended to evaluate any changes in the cyst and monitor bone healing.
Disclaimer: This report provides a reference for medical imaging analysis and does not replace in-person consultation or professional medical advice. Specific treatment plans should be individualized according to the patient’s actual condition under the guidance of a specialist.
Human Doctor Final Diagnosis
Solitary/Unicameral/Juvenile Bone Cyst (SBC)