Avulsed bipartite patella in 19-year-old woman with anterior knee pain



Clinical History
A 19-year-old female patient was referred with anterior knee pain and a palpable hard mobile mass above the patella. Her medical history included a twisting injury 4 years prior to imaging. No ecchymosis or bruising was observed clinically. MR imaging was suggested.
Imaging Findings
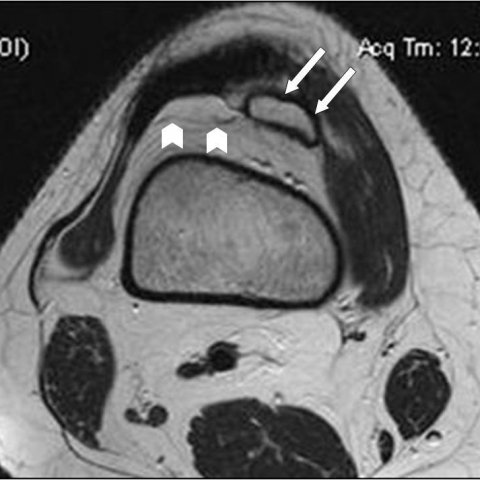
MR imaging was performed with a 1.5 Tesla scanner using standard sequences. Axial T2-w (Fig. 1), sagittal PD (Fig. 2) and coronal T1-w images (Fig. 3) demonstrated an osseous fragment located posterosuperiorly and medially to the upper pole of the patella. There was also a small amount of intra-articular fluid (Fig. 1, 3). The coronal fat suppressed PD-w (Fig. 4) MR image, showed the presence of bone marrow oedema within the patella at the site of the avulsed bipartite fragment.
Discussion
A. Patella is the largest sesamoid in the body [1]. It is a cartilaginous structure, which begins to ossify at 3 years of age from its centre to periphery until the age of 6 [2]. At the age of 12, secondary ossification centres develop and they are fused in adolescence. If this process is not completed, a bipartite patella results [1]. Bipartite patella is a normal developmental variant of the ossification centres, occurring in 1−2% of the general population and is more common in men [1, 3, 4]. Pathophysiology of this entity is not clear yet. Some authors suggest that bipartite patella is the result of repetitive microtrauma due to abnormal mobility at the fibrocartilaginous interface between ossification centres [1]. Other authors consider that there is non-union of disseminated ossification centres due to stress at the insertion site of the vastus lateralis [3]. Rarely, a tripartite or multipartite patella may be seen.
B. This entity is usually asymptomatic and is frequently discovered incidentally [2]. However, a painful bipartite patella in adolescents and young adults has been described [4]. The cause of pain is due to mobility of the synchondrosis between the patella and the bipartite fragment. MRI is important in this respect, because it reveals the presence of bone marrow oedema and explains the localised tenderness [1, 4]. A traumatic separation of a bipartite patella has been reported as rare complication [5]. Migration of the avulsed fragment, as shown herein, is extremely rare.
C. This entity could be recognised with X-rays, MR imaging or computed tomography. MR imaging is the gold standard for diagnosing symptomatic patients presenting with anterior knee pain, as it depicts the bone marrow oedema and the peripatellar soft tissue oedema. It has been reported that scintigraphy could be an alternative option of MRI [2]. A migrated avulsed fragment can easily be depicted with all imaging modalities. Imaging is important in differentiating a traumatic fracture from bipartite patella, the later showing irregular corticated borders.
D. Treatment of bipartite patella is usually conservative with nonsteroidal anti-inflammatories and physiotherapy and the prognosis is very good. In patients with persisting symptoms, surgical retinacular release, resection of the fragment with subsequent tendinous reattachment are the treatment options [2]. In our patient, the treatment included surgical reattachment and fusion of the fragment.
E. Bipartite patella may be complicated by avulsion of the fragment and may simulate the presence of a knee joint mass.
Differential Diagnosis List
Final Diagnosis
Avulsed bipartite patella presenting as mass causing anterior knee pain.
Liscense
Figures
MR axial image
MR sagittal image

MR coronal image

MR coronal image

Medical Imaging Analysis Report
I. Imaging Findings
The patient is a 19-year-old female presenting with anterior knee pain and a palpable hard mass with good mobility located above the patella. Based on the provided MRI images, the following findings are noted:
- A relatively intact separated bone fragment with pronounced sclerotic edges is located at the superior pole of the patella near the patellar tendon attachment (indicated by the arrow).
- There is a separation between the fragment and the main body of the patella, accompanied by localized soft tissue swelling or synovial thickening.
- Mild bone marrow edema signals may be present (especially in the bone fragment and the adjacent patellar edge), suggesting inflammation/edema caused by repetitive traction or strain.
- No significant large hematoma or tear is evident in the surrounding soft tissues, but localized signal changes and minor effusion are seen.
II. Possible Diagnoses
Based on the above imaging findings and clinical history, the following diagnoses or differential diagnoses should be considered:
- Bipartite Patella with Local Avulsion: Bipartite patella is a normal variant in patellar development, but separation of the bone fragment or pain symptoms can occur under trauma or repetitive traction stress. Imaging typically shows sclerotic margins of the fragment with continuous yet separated cortical bone.
- Fracture/Avulsion Fracture of the Patella or Patellar Tendon Attachment: Unlike bipartite patella, a true acute fracture typically has sharper edges and a clear fracture line, with a lack of sclerotic margins around the fragment. If trauma occurred long ago, thicker encapsulation or sclerosis may appear.
- Loose Body: Usually seen after cartilage or osteochondral injuries, often accompanied by other intra-articular cartilage lesions. This should be considered if there is a relevant history or other joint pathology.
III. Final Diagnosis
Considering the patient's age, anterior knee pain, a palpable mobile bony mass, and the MRI findings of a separated bone fragment with sclerotic borders and mild edema at the superior pole of the patella, the most likely diagnosis is: “Bipartite Patella with an Avulsed Bone Fragment Displacement.” This diagnosis is consistent with literature reports and represents a rare complication of bipartite patella caused by chronic wear or trauma.
IV. Treatment Plan and Rehabilitation
For bipartite patella that is asymptomatic or mildly symptomatic, conservative treatment is generally adopted. However, in this case, due to a clearly detached or displaced fragment accompanied by pain, surgical intervention may be considered. The specific treatment plan may include the following steps:
- Conservative Treatment:
- Rest and temporarily avoid excessive weight bearing: reduce running, jumping, and squatting to alleviate pain.
- Oral NSAIDs to lessen local inflammation and pain.
- Use a knee brace or support for local stability.
- Physical therapy (e.g., ultrasound, low-frequency electrical stimulation) to help reduce soft tissue edema and pain.
- Surgical Treatment:
- If conservative management fails and the bone fragment is obviously displaced, refixation or excision of the fragment with repair of the ligament attachment may be performed.
- For larger bone fragments causing recurrent pain or joint dysfunction, fixation using screws or absorbable devices can be performed to achieve reintegration.
- Postoperatively, gradually start rehabilitation exercises based on the recovery progress.
Rehabilitation and Exercise Prescription Recommendations (FITT-VP Principle):
- Frequency (F): Initially 3–4 times per week, avoiding excessive fatigue and high-impact activities.
- Intensity (I): Begin with low-resistance or bodyweight exercises, gradually increasing the resistance (e.g., resistance bands).
- Time (T): 20–30 minutes per session, including warm-up, exercise, and stretching.
- Type (T): Emphasize non-weight-bearing or low-impact exercises, such as straight leg raises, isometric contraction exercises for the knee, and wall sits. Progress to stationary cycling or swimming as joint-friendly options.
- Progression (P): Gradually increase exercise intensity and duration based on pain levels and muscle strength recovery, ensuring no significant pain or discomfort arises.
Individualization is key. If severe knee pain or fragment instability persists, reduce or pause weight-bearing training until inflammation subsides, then resume exercise.
Disclaimer: This report is a reference-based analysis based on current imaging and clinical data and does not replace an in-person consultation or professional medical advice. If you have any doubts or if your symptoms worsen, please seek medical attention promptly.
Human Doctor Final Diagnosis
Avulsed bipartite patella presenting as mass causing anterior knee pain.