Pigmented villonodular synovitis of the shoulder



Clinical History
A 32-year-old male patient presented with a 1-year history of spontaneous shoulder pain. Physical examination revealed shoulder stiffness.
Imaging Findings
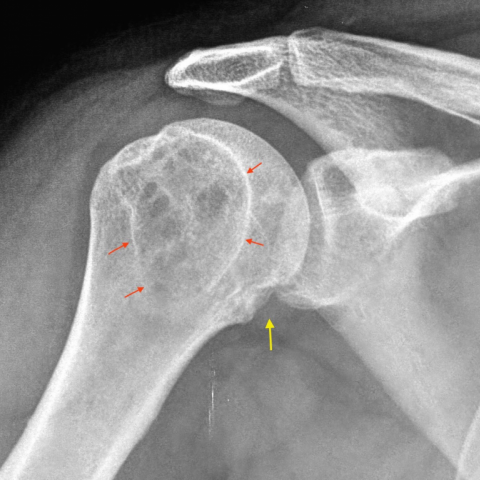
Plain radiograph demonstrated intraosseous cystic lesions and articular erosions in the humerus head (Fig. 1a).
CT shows better the well-defined lytic areas with sclerotic rim together with chronic degenerative changes such as decrease of the joint space and sclerosis (Fig. 1b). No calcifications were seen.
Coronal FSE PD-WI with and without fat saturation (Fig. 2a, b) and axial FSE T2-WI (Fig. 3a, b) showed nodular synovial intraarticular masses of marked low signal intensity (Fig. 4a, b), extending to the long biceps tendon sheath and axillary recess. Cystic osseous erosions and degenerative changes in the glenohumeral joint were also present.
Discussion
Intraarticular giant cell tumour (GCT), also known as pigmented villonodular synovitis (PVNS), is an uncommon benign proliferative process affecting synovial membranes (and can thus also include bursae and tendons).
Depending on the site of origin, it can be divided into iintraarticular or extraarticular and depending on the pattern of growth localized or diffuse. It typically affects patients of 20-50 years of age, with equal frequency in men and women.
The cause of PVNS is not known. Microscopically synovial hyperplasia is accompanied by organizing surface fibrin deposits, stromal fibrosis, chronic inflammation, and generally accumulations of macrophages that often contain cytoplasmic haemosiderin pigment.
Diffuse GCT is usually a monoarticular process of large joints with the knee being the most common (66-80%), followed by the hip, ankle, shoulder [3, 4] and elbow, in descending frequency. Localized intra-articular type of GCT or PVNS occurs almost exclusively within the knee [1, 7].
Our case shows unusual presentation in the shoulder with large bone erosions [4].
Most cases come with joint swelling, pain and occasionally joint dysfunction.
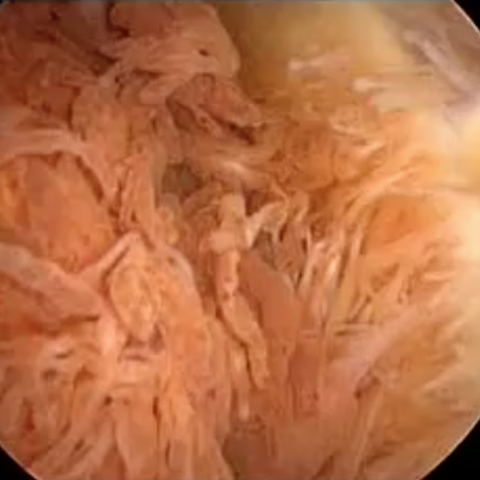
Hypertrophic synovium may appear villous, nodular, or villonodular with prominent haemosiderin deposition. Most patients have a haemorrhagic, dark brown synovial fluid.
Biopsy is diagnostic [5].
Plain radiographs may be normal, show periarticular soft tissue swelling and local osseous changes such as extrinsic bone erosions, osteopaenia, joint space narrowing, intraarticular osteochondral bodies and degenerative disease (Fig. 1a) [1].
CT can show joint effusion, erosions and bone cysts and intraarticular soft tissue mass of synovial tissue, sometimes slightly hyperdense compared to muscle (Fig. 1b).
MRI is the best imaging technique for the diagnosis of GCT. Synovial thickening in MRI characteristically shows intermediate to low signal intensity on T1-WI and markedly low on T2-WI MR-images, due to T2-relaxation time shortening caused by haemosiderin deposits together with collagen bundles. This effect is accentuated on gradient-echo images, the so-called “blooming” effect, caused by increased magnetic susceptibility artefact (nearly pathognomonic of pigmented villonodular synovitis) [5]. Other MRI findings include bone erosion, subchondral cysts, bone marrow oedema and cartilaginous defects (Fig. 2, 3). Marked enhancement of the synovium is common after gadolinium injection.
Treatment usually consists of surgery (synovectomy). Both arthroscopic and open surgery can be used. However, there is a high rate of recurrence, especially on diffuse forms. Adjuvant treatment is often employed, especially in recurrent cases, external beam radiotherapy or new treatments with tyrosine kinase inhibitors [6]. In cases of extensive joint destruction total joint replacement is the best procedure.
Differential Diagnosis List
Final Diagnosis
Diffuse type of GCT of the shoulder
Liscense
Figures
Radiografía y TC

RM de hombro, plano oblicuo coronal


RM de hombro, plano axial


Artroscopia

Medical Imaging Analysis Report
I. Imaging Findings
1. X-ray (Figure 1): Localized multiple osteolytic or erosive lesions (indicated by red arrows) can be seen in the humeral head, with irregular margins and a noticeable soft tissue shadow. The joint space is still present, but a slight narrowing of the local joint space is observed (indicated by yellow arrows).
2. CT Scan (Figure 2): A soft tissue mass (red arrow) is seen within the shoulder joint cavity, adjacent to the humeral head and the glenoid. Evident bone erosion or cystic changes can be observed; the margins of the bony destruction are relatively clear (yellow arrow).
3. MRI Examination (Figures 3, 4, 5, 6): On T1-weighted images, the lesion predominantly appears as intermediate to low signal; on T2-weighted and gradient echo sequences, it demonstrates a significantly low signal with evident “blooming” artefact. In some areas, there is bone erosion or tumor-like extension, along with mild bone marrow edema. Post-contrast images show heterogeneous enhancement, suggesting thickened synovial tissue and possible solid components.
4. Arthroscopic Findings (Figures 7, 8): Proliferative synovial tissue is visible within the joint cavity, exhibiting a brownish-yellow color, with a flocculent or villous appearance, consistent with gross findings of hemosiderin deposition.
II. Potential Diagnoses
1. Pigmented Villonodular Synovitis (PVNS): Also known as giant cell tumor or synovial giant cell tumor, often involves a single joint. Imaging may show an intra-articular soft tissue mass, bone erosion, and low-signal areas (caused by hemosiderin). Histologically, synovial proliferation and hemosiderin deposition are common.
2. Synovial Chondromatosis: Typically characterized by local or loose chondral bodies or ossified nodules. On MRI, multiple cartilage nodules with peripheral calcifications can be seen. The absence of obvious calcification in this case does not completely match synovial chondromatosis.
3. Other Inflammatory or Neoplastic Joint Lesions: Such as inflammatory arthritis (rheumatoid arthritis, gouty arthritis, etc.) or malignant synovial tumors. These usually have corresponding inflammatory or other specific features (e.g., severe osteoporosis or a large amount of joint effusion) which are not entirely consistent with this case when considering both imaging and clinical history.
III. Final Diagnosis
Considering the patient’s age of 32, spontaneous shoulder pain, restricted joint mobility, the imaging findings of intra-articular soft tissue mass, bone erosion, and low signal with “magnetic susceptibility” on MRI, along with arthroscopic evidence of brownish-yellow villous synovial proliferation, the most likely diagnosis is: Pigmented Villonodular Synovitis (PVNS).
IV. Treatment Plan and Rehabilitation
1. Treatment Options:
- Surgical Treatment: Mainly arthroscopic or open synovectomy (i.e., synovial debridement/synovectomy). For localized or diffuse lesions, surgery helps relieve pain, improve function, and slow further joint destruction.
- Adjuvant Therapy: If there is a risk of incomplete resection or recurrence after surgery, radiotherapy or novel treatments such as tyrosine kinase inhibitors may be considered, depending on the extent of the lesion and pathological type.
- Joint Replacement: In cases of severe joint destruction or advanced disease, joint replacement may be performed to relieve symptoms and restore function.
2. Rehabilitation and Exercise Prescription (FITT-VP principle):
- Early Postoperative Stage (1–4 weeks):
· Focus on pain relief and controlling inflammation; range-of-motion exercises should be within the pain-tolerable range.
· Perform gentle passive or assisted-active exercises 2–3 times daily, each session lasting 5–10 minutes.
· Avoid excessive loading and vigorous exercises to protect the surgical site during healing.
· Under the guidance of a physician or rehabilitation therapist, perform passive shoulder mobilization exercises and use pulleys or support devices to assist lifting.
- Mid-Term Rehabilitation (4–8 weeks):
· Gradually increase active range-of-motion training, combined with isometric or low-resistance isotonic exercises for the shoulder girdle muscles.
· Progress from bodyweight exercises to light-to-moderate resistance band exercises, 3–4 times per week, 15–20 minutes per session.
· Incorporate shoulder stability and balance exercises, such as using small balls or lightweight dumbbells for shoulder external rotation, internal rotation, and other targeted muscle training.
- Late Rehabilitation (after 8 weeks):
· Emphasize joint stability and functional recovery, gradually returning to normal daily activities or sports.
· Under the supervision of a rehabilitation therapist, progressively increase resistance and loading to strengthen the rotator cuff muscles (supraspinatus, infraspinatus, teres minor, subscapularis) at least 3 times per week.
· If the patient has higher functional or sports needs, more intense functional training (e.g., swimming or resistance band drills) can be introduced approximately 3 months postoperatively.
- Individualization and Safety: Throughout the rehabilitation program, adjustments should be made based on the patient’s pain tolerance, swelling response, and joint stability. In cases of fragile bone or other comorbidities, exercise intensity should be reduced, and cardiopulmonary function should be monitored. Cardiorespiratory endurance training can be incorporated if necessary.
Disclaimer:
This report is based on current clinical and imaging data for reference only and does not replace an in-person consultation or professional medical opinion. Specific diagnosis and treatment plans should be determined by combining the patient’s actual condition and following the guidance of a specialist.
Human Doctor Final Diagnosis
Diffuse type of GCT of the shoulder