Giant cell tumour of sacrum



Clinical History
17-year-old male patient presented with progressively increasing low back pain and numbness in the toes of the right foot for the past 2 months. MRI of lumbosacral spine without gadolinium was obtained as screening investigation.
Imaging Findings
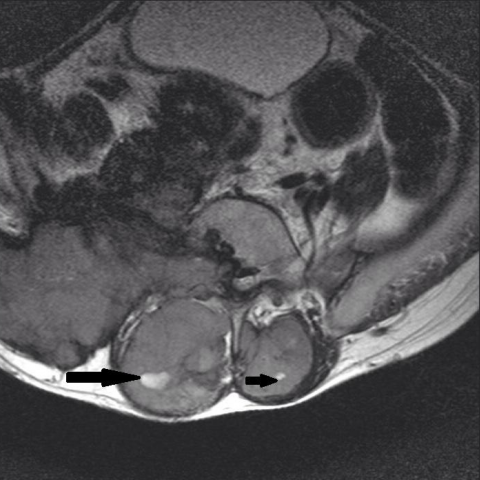
MRI revealed a large expansile lesion with extensive soft tissue component arising from sacral vertebrae and both sacral alae (Fig. 1). The mass showed heterogeneous low to intermediate signal intensity on T2WI with curvilinear area of low signal intensity on T1WI and T2WI (Fig. 2). Few small foci of high intensity on T2WI and STIR sequence were seen within the soft tissue mass in keeping with cystic or necrotic components. As the imaging findings were suggestive of a neoplastic mass of the sacrum, surgical biopsy and histopathological analysis were performed. Microscopy showed a neoplastic lesion composed of evenly dispersed giant cells interspersed with proliferating mononuclear stromal cells. Occasional mitosis was found. Findings were consistent with giant cell tumour.
Discussion
Giant Cell Tumour (GCT) is a relatively common skeletal tumour, accounting for 4%–9.5% of all primary osseous neoplasms and 18%–23% of benign bone neoplasms. GCT is typically benign and solitary. However, multiple lesions have been described and 5%–10% of lesions may be malignant. [1] It occurs most commonly in 3rd to 5th decades of life and affects both males and females with slight female preponderance. [2] The most common specific location of GCT is about the knee. The single most common site is the distal femur followed by the proximal tibia, distal radius, sacrum (4%–9%) and proximal humerus. [1]
Sacral lesions are frequently large with destruction of the sacral foramina, but this nonspecific finding is also observed with other large sacral lytic lesions. A sacral GCT commonly involves both sides of the midline, and an extension across the sacroiliac joint is frequent. This feature is infrequent in GCT of long bone as the epiphysis serves as barrier and limits invasion of the joint. [3] CT improves detection of cortical thinning, pathologic fracture, periosteal reaction and degree of osseous expansile remodelling compared with radiography. [1]
MRI of a GCT often show heterogeneous signal intensity on all pulse sequences. Generally, the tumour is of low to intermediate signal intensity on T1-weighted images (WI). Interestingly, GCT have low to similar signal intensity to the normal spinal cord on T2-WI. This reflects the relative collagen content of fibrous components and haemosiderin within the tumour. Although this feature is not unique to giant cell tumours of the spine, it is quite helpful in making a differential diagnosis because most other sacral neoplasms (metastases, myeloma, lymphoma and chordoma) show high signal intensity on the long-TR MR images. This appearance may be the initial imaging characteristic suggestive of a correct diagnosis. Evidence of recent haemorrhage may also be apparent with areas of high signal intensity on T1-WI and T2-WI or fluid–fluid levels on the MR images. Cystic areas (similar to those seen in aneurysmal bone cyst) and regions of old haemorrhage with haemosiderin deposits are common. [3] Intralesional curvilinear areas of low signal intensity have also been described previously in plasmacytoma and vertebral haemangioma. [4] A solitary bone plasmacytoma needs to be considered in a differential diagnosis. However, heterogeneous signal intensity on T2-WI heterogeneous enhancement, and cystic changes are unusual in vertebral haemangioma. [3] GCT shows a variable degree of enhancement on post contrast study. The patient is offered radiation therapy as large expansile sacral mass is amenable to complete excision.
Differential Diagnosis List
Final Diagnosis
Giant cell tumour of sacrum
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Axial image of lumosacral spine, expansile mass from sacrum


MR, Sagittal images of lumbosacral spine



1. Imaging Findings
Based on the provided MRI (lumbar-sacral spine routine sequence, without contrast), the following findings are noted:
• The lesion is located in the sacrum, showing a large area of lytic and expansile changes involving multiple segments of the sacral vertebrae, crossing the midline.
• On T1WI, the lesion predominantly shows low to intermediate signal. On T2WI, it also appears as relatively low to intermediate or slightly mixed signal, and some areas show inhomogeneity (indicating possible scar tissue, hemorrhage, or cystic changes).
• The cortical bone of the sacral vertebra is thinned and partially destroyed, possibly affecting or compressing adjacent nerve pathways (e.g., through the anterior sacral foramen or within the spinal canal). The patient reports toe numbness, which may be related to nerve compression at the corresponding segments.
• A soft tissue component is observed with possible cystic or hemorrhagic regions internally (inferred from a few high-signal areas).
2. Differential Diagnoses
Based on the patient’s age, clinical symptoms, and imaging findings, the following differential diagnoses should be considered:
- Giant Cell Tumor (GCT) of the Sacrum: Commonly seen in patients aged 20–40 but can also occur in younger individuals. Typically presents as a lytic, expansile lesion involving the epiphysis, often crossing the articular surface. On MRI, GCT usually shows low to intermediate signal on T1WI and low to intermediate signal on T2WI, which is a key characteristic.
- Spinal Metastasis: Relatively rare in a 17-year-old, and usually accompanied by a known primary tumor. They often appear hyperintense on T2WI, with bone destruction and an accompanying soft-tissue mass within the spinal canal.
- Solitary Plasmacytoma of the Spine or Sacrum: May present as a lytic lesion, though less common in younger individuals. MRI findings can be heterogeneous on T2WI, often with prominent enhancement. Clinically, there may be associated serological abnormalities (e.g., immunoglobulin changes).
- Chordoma: Often found in the sacral base or coccyx region. On MRI, chordomas typically exhibit high signal on T2WI due to mucinous components, which differs somewhat from this case of predominantly low to intermediate T2 signal.
3. Final Diagnosis
Taking into account the patient’s age (17 years), progressively worsening lumbosacral pain and toe numbness, and MRI findings of a lytic, expansile lesion showing low signal on T1WI and low to intermediate signal on T2WI, the most consistent diagnosis is:
Giant Cell Tumor of the Sacrum.
Pathological confirmation is still essential; if further confirmation is needed, a biopsy or surgical pathology examination is recommended.
4. Treatment Plan and Rehabilitation Program
Treatment Strategy:
• Surgical Treatment: If the lesion is localized and can be completely excised, surgery is the first choice. Possible procedures include partial sacrectomy or curettage, followed by bone grafting or reconstruction.
• Radiation Therapy: For extensive lesions that cannot be completely excised or when surgery poses a high risk, consider radiotherapy or a combination of surgery and radiotherapy.
• Medication: Use of bisphosphonates or other agents may help control pain and disease progression. Targeting the RANKL pathway (e.g., denosumab) may be considered, especially when surgical intervention is difficult.
Rehabilitation and Exercise Prescription:
- Rehabilitation Principles: Focus on protecting the treated area and relieving symptoms while gradually strengthening core and lower-limb muscles. Avoid excessive loading and reinjury.
- Initial Stage (Preoperative or Acute Pain Phase):
- Avoid heavy loading on the lumbosacral region and repetitive flexion movements.
- Engage in gentle core stabilization exercises, such as supine abdominal drawing-in or slight posterior pelvic tilt, holding for 5–10 seconds per repetition, 2–3 sets per day, with 5–10 repetitions per set.
- Perform light walking or use assistive devices to reduce pain and burden.
- Recovery Stage (Postoperative or Reduced Symptoms):
- Once the surgical site has healed and with medical approval, gradually increase core, hip, and knee strengthening exercises (e.g., straight leg raises, bridging). Perform 2–3 sets each session, with 10–15 repetitions per set, adjusting intensity according to tolerance.
- Progress to low-intensity aerobic activities (e.g., swimming, stationary cycling) 3–4 times per week, each session lasting 20–30 minutes.
- Later Consolidation Stage:
- In the absence of significant pain or radicular symptoms, transition to moderate-intensity core stabilization (e.g., plank, side plank) and lower-limb weight-bearing exercises (e.g., half squats, partial weight-bearing drills) at least 3 times weekly.
- Focus on comprehensive training of core, back, and both lower limbs to improve flexibility, strength, and coordination, gradually returning to normal physical activities.
- Individualization and Safety: Throughout the rehabilitation process, adjust exercise load according to the patient’s tolerance to pain and activity. Follow the FITT-VP principle (Frequency, Intensity, Time, Type, Volume, and Progression). If pain or neurological symptoms worsen, seek medical advice promptly.
5. Disclaimer
This report is formulated based on currently available imaging and medical history data for reference only and does not substitute for an in-person consultation or professional diagnosis and treatment plan. Actual diagnosis and treatment require combining clinical presentation, laboratory tests, and pathological results. Patients should visit the relevant specialist as soon as possible and adhere to individualized medical advice.
Human Doctor Final Diagnosis
Giant cell tumour of sacrum