

An 87-year-old female patient presented without symptoms for follow-up imaging after treatment for uterine cervix carcinoma including hysterectomy, radiation therapy with 45Gy (weekly fractionation 5 x 1.8Gy) and intracavitary HDR-Brachytherapy (2 x 5Gy). Lab parameters were unremarkable.
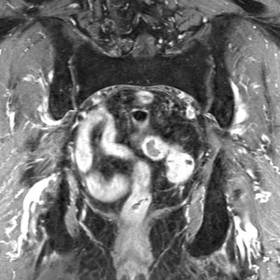
No osseous signal changes are visible in MRI 6 weeks after radiation therapy compared to the previous imaging (Fig. 1). Eight months after therapy, there was a minor focal but also diffuse gadolinium uptake adjacent to the left sacroiliac joint (SIJ) and new, spotted signal changes on the T1w-image adjacent to the right SIJ (Fig. 2).
After 18 months, nearly the entire sacrum showed a massive T1w signal increase following contrast administration with a central hypointense area and a peripheral hyperintense signal on the right side of the sacrum (Fig. 3a). There was also a fine hypointense line parallel to the left SIJ, interpreted as an insufficiency fracture (Fig. 3b).
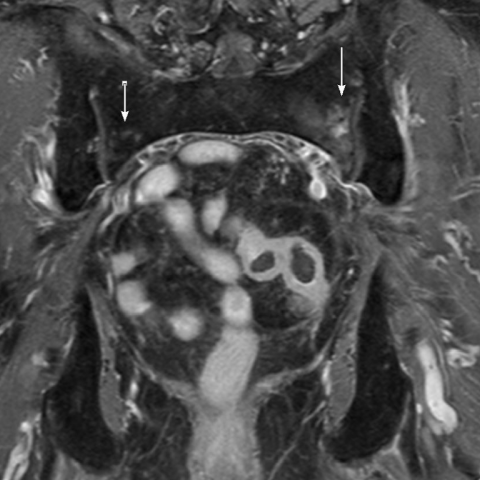
After 40 months, MRI post-Gadolinium demonstrated decreased signal alterations as well as smaller lesions with a circular hyperintense rim and an iso-/hypointense centre on the right (Fig. 4). On the axial T1w image after contrast there were no visible lines suspicious for persistent fractures.
Adverse reactions in healthy, tumor-unaffected tissues are common side effects in the context of radiotherapy (Dalinka et al 1985). The major adverse event of, usually attenuated, irradiation of healthy bone tissue is osteoradionecrosis (ORN). The incidence ranges from 2.1-34% according to literature (Feltl et al 2006). ORN results, inter alia, by vascular damage and damage in bone remodelling cells such as osteoblasts, which often lead to increased cell death (Burgener et al 1991). The extent of vascular damage, the diminished osteoblastic activity and thus the risk for osteonecrosis depends on several factors. Primary causes are treatment-related factors such as the type of irradiation (external radiation and / or brachytherapy), duration and fractionation of the radiation therapy, the total dose of radiation and finally additional potentially toxic therapies such as chemotherapy. Also, the extent of the radiation response depends on individual patient factors such as the patient’s age, comorbidities, already preexisting osteopenia, as well as additional medication such as steroids (Mitchell et al 1998).
One sequalae of ORN in the sacrum, which is most commonly affected, is progressive biomechanical bone instability leading to insufficiency fractures. The extent of insufficiency fracture is often subtle (Howland et al 1975). Differential diagnosis to metastatic disease or reactive changes may be difficult. Insufficiency fractures often present in T1-weighted images as fine hypointense lines parallel to the SIJ. Important points to distinguish benign from malignant lesions or masses are the symmetry and the distribution pattern, both, in the entire body as well as in the irradiated bone. While metastases generally occur in an asymmetrical distribution and frequently multiple lesions are to be found, ORN demonstrate frequently as symmetrical, often bilateral lesions in the radiation-exposed area of the pelvis (Ugurluer et al 2014). Furthermore, secondary sarcomas are rare after radiotherapy and usually occur after a longer latency period of many years following radiation treatment. These lesions show a progressive osteodestructive pattern. Osteoradionecrosis show both, a morphologically and temporally heterogeneous, individual course due to risk factors (osteopaenia, chemotherapy etc.) and complications such as non-/slow healing insufficiency fractures. Often the necrosis is self-limited. Uniform and/or guideline-related treatments do not exist. In conclusion, the above-mentioned radiological changes such as symmetry, sequelae of reversible osseous signal changes and the absence of metastastic evidence within the context of radiation therapy strongly suggests that the findings are conclusive for a combination of reactive inflammatory bone marrow response, radiation-induced osteonecrosis, insufficiency fractures and increased bone remodelling.
Healing osteoradionecrosis with secondary insufficiency fracture.
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.







According to the provided MRI sequences, symmetrical abnormal signal changes are observed in the pelvic region (primarily involving the sacrum, ilium, and surrounding bony structures), presenting as follows:
Overall, these imaging changes indicate radiation-induced osteoradionecrosis (ORN) in the irradiated skeletal regions, accompanied by minimal or unstable fractures (often referred to as insufficiency fractures).
Considering the patient’s advanced age, previous surgery and radiotherapy for cervical cancer, symmetrical bony signal changes on imaging, incomplete fractures, and lack of evidence of active malignancy or infection, the most likely diagnosis is:
“Radiation-induced osteoradionecrosis (ORN) with insufficiency fractures of the sacrum and pelvis.”
Given that the patient currently has no significant symptoms and normal lab results, radiation-induced osteoradionecrosis should be primarily considered. Close follow-up and symptomatic treatment are advised.
For elderly patients at risk of radiation-induced osteoradionecrosis and incomplete fractures, the key principles of rehabilitation are safety, gradual progression, and individualization:
During rehabilitation, closely monitor any changes in pain, mobility, and gait stability. If new or worsening pain or signs of a possible fracture occur, revisit a physician promptly and adjust the plan accordingly.
This report is based on the current imaging and medical history available and serves as a reference for medical analysis. It cannot fully replace in-person consultations or professional medical advice. If there are any questions or changes in symptoms, please seek medical attention promptly.
Healing osteoradionecrosis with secondary insufficiency fracture.