A ganglion cyst causing tarsal tunnel syndrome



Clinical History
A 42-year-old male with no comorbidities presented with complaints of pain on the medial aspect of the left ankle, cramps on the left leg during the night and numbness of the left first to third toes for 4 weeks.
On clinical examination, he had normal power of intrinsic foot muscles with normal sensation. Tinel’s sign was positive in the left tarsal tunnel region along with tenderness.
Imaging Findings
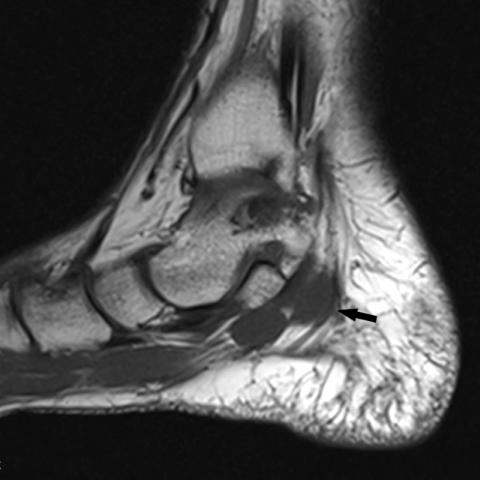
MRI of the left ankle shows a lobulated mass along the medial aspect of the calcaneus (arrow), demonstrating fluid signal intensity on fat-suppressed T2-weighted sagittal (Figure 1a) and coronal (Figure 1b) images and T2-weighted sagittal image (Figure 1d). The mass demonstrated an iso to hypointense signal intensity to skeletal muscle on T1-weighted images (Figure 1c) along the medial aspect of the calcaneum posterior to the flexor digitorum longus tendon.
Ultrasound of the left ankle shows a lobulated cystic lesion behind the medial malleolus (Figure 2).
Discussion
Background
The tarsal tunnel is a fibro-osseous channel extending from the ankle to the midfoot, through which the medial tendons and the posterior tibial neurovascular bundle pass. Tarsal tunnel syndrome (TTS) is a compression neuropathy of the posterior tibial nerve or one of its branches and may be caused by a variety of pathologic lesions [1].
The aetiology can be intrinsic or extrinsic:
- Extrinsic causes include poorly fitting shoes, trauma, anatomic-biomechanical abnormalities (tarsal coalition, valgus or varus hindfoot), post-surgical scarring, systemic diseases, generalised lower extremity oedema, systemic inflammatory arthropathies, diabetes, and post-surgical scarring.
- Intrinsic causes include tendinopathy, tenosynovitis, perineural fibrosis, osteophytes, hypertrophic retinaculum, and space-occupying or mass effect lesions (enlarged or varicose veins, ganglion cyst, lipoma, neoplasm, and neuroma). Arterial insufficiency can lead to nerve ischemia [3].
Clinical Perspective
Symptoms include sole numbness, pain, and a cold sensation; they affect the patient’s quality of life [2]. TTS can present similarly to other lower extremity conditions, with the most common differential diagnosis being plantar fasciitis, as these patients also present with plantar heel pain. In addition to plantar fasciitis (in which TTS is thought to be commonly misdiagnosed), polyneuropathy, L5 and S1 nerve root syndromes, Morton’s metatarsalgia, compartment syndrome of the deep flexor compartment will have to be distinguished from tarsal tunnel syndrome as well [4].
Imaging Perspective
Imaging, in particular MRI, can help identify causative factors in individuals with suspected TTS and help aid surgical management. The detection of a space-occupying lesion is important, as surgery is advised.
Outcome
Treatment of tarsal tunnel syndrome is initially conservative and includes behavioural modification, physical therapy, immobilisation, and anti-inflammatory medication. Surgical release of the flexor retinaculum and removal of the offending mechanism is attempted in refractory cases or in cases with mass effect, but results vary depending on the aetiology, duration of symptoms, and the age of the patient. The longer the duration of symptoms and the older the patient, the worse the prognosis.
Take Home Message / Teaching Points
- To consider tarsal tunnel syndrome in paraesthesia of the foot.
- There is no best test to diagnose tarsal tunnel syndrome, and it is a combination of history, examination, imaging, electromyography and nerve conduction studies.
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Ganglion cyst causing tarsal tunnel syndrome
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures




Medical Imaging Analysis Report
I. Imaging Findings
Based on the provided MRI images, there is an irregular cystic or cyst-like high-signal lesion located near the medial malleolus of the left foot (in the tarsal tunnel region where the posterior tibial nerve runs). Surrounding tissue structures are locally compressed. This cystic structure is adjacent to the flexor retinaculum and surrounding soft tissues, and the signal characteristics suggest a fluid component. Mild soft tissue edema or inflammatory signs are visible in the surrounding area, but there is no obvious abnormality in the local bone.
II. Potential Diagnoses
- Tarsal Tunnel Syndrome (TTS)
Rationale: The patient’s symptoms are concentrated around the medial malleolus area, including nighttime cramping and toe numbness, and Tinel’s sign (tapping test) is positive. MRI suggests a cystic lesion in the tarsal tunnel region that may be compressing the posterior tibial nerve. - Plantar Fasciitis
Rationale: The patient experiences foot pain, with heel pain being common. However, in this case, pain in the medial malleolus region and nerve numbness, along with a cystic lesion in the medial malleolus, make TTS more likely. Plantar fasciitis should be ruled out. - Other Ankle or Foot Nerve Entrapment Disorders
This includes peripheral neuritis or space-occupying lesions (such as schwannomas, ganglion cysts, etc.). Further investigation is required to exclude other neurogenic pathologies.
III. Final Diagnosis
Considering the patient’s symptoms (medial malleolus pain, toe numbness, nighttime cramping), clinical examination findings (positive Tinel’s sign), and imaging findings (cystic lesion in the tarsal tunnel region likely compressing the posterior tibial nerve), along with no significant history of other systemic diseases, the most likely diagnosis is: Tarsal Tunnel Syndrome of the Left Foot (potentially caused by a cystic lesion such as a ganglion cyst).
IV. Treatment Plan and Rehabilitation
1. Conservative Treatment
- Pressure Reduction and Symptom Management: It is recommended to wear loose, well-fitted shoes and avoid prolonged standing or weight-bearing. Using arch supports or foot pads may help improve foot load distribution.
- Medication: Non-steroidal anti-inflammatory drugs (NSAIDs) may be considered to reduce local inflammation and pain, under the guidance of a physician.
- Physical Therapy: This may include ultrasound therapy, local cold or heat therapy, and gentle massage to alleviate tension and local inflammation.
- Orthotic Devices and Immobilization: An ankle brace may be considered at night to maintain proper alignment and reduce nerve compression.
2. Surgical Indications
If conservative treatments fail or MRI confirms a significant space-occupying lesion (e.g., cystic or tumorous mass) causing prolonged nerve compression, surgical decompression and/or excision of the cyst may be considered. Surgical outcomes depend on factors such as the patient’s age, duration of symptoms, and the specific etiology.
3. Sample Rehabilitation/Exercise Prescription
Rehabilitation should be conducted progressively, following the FITT-VP principle:
- Frequency (F): 3–4 times per week, adjusted flexibly based on soft tissue recovery.
- Intensity (I): Start with low-intensity training; discontinue or adjust immediately if pain or discomfort occurs.
- Time (T): About 20–30 minutes per session initially, which can gradually be increased to 30–45 minutes.
- Type (T):
- Ankle Range of Motion Exercises: For example, ankle circles, flexion, and extension.
- Muscle Strengthening: Use a resistance band for gentle plantarflexion and dorsiflexion exercises, ensuring controlled movements.
- Balance and Proprioception Training: Gradually attempt single-leg standing or use a balance board, avoiding excessive weight-bearing.
- Progression (P): As symptoms improve, gradually increase training difficulty, such as by extending exercise time or using higher resistance bands. However, avoid excessive foot fatigue.
Notes: If the patient experiences significantly increased pain, foot swelling, or marked discomfort at night, seek medical attention or adjust the training regimen promptly.
Disclaimer: This report serves as a reference analysis and does not substitute for an in-person consultation or professional physician’s advice. If you have any questions, please consult your clinical doctor promptly.
Human Doctor Final Diagnosis
Ganglion cyst causing tarsal tunnel syndrome