Sciatic nerve palsy complicating posterior hip dislocation in a child



Clinical History
The patient was pushed down when playing soccer. He felt an acute pain at the right hip; the right thigh was flexed, adducted and intra-rotated on physical examination. Posterior hip dislocation was diagnosed; after closed reduction of the hip dislocation the patient showed neurological deficit in the L4-S1 distribution territory.
Imaging Findings
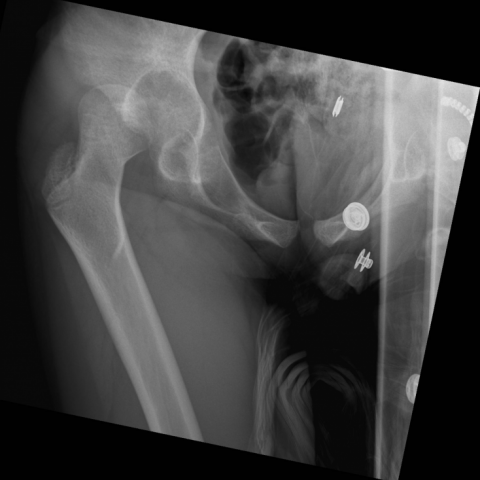
Plain film showed cranial dislocation of the right femoral head (Fig. 1). CT revealed cranial and posterior hip displacement but no fracture and a doubtful damage of the acetabular physeal cartilage (Fig. 2). Closed reduction was successfully performed under general anaesthesia (Fig. 3). MRI performed one week later showed a fluid collection close to the right aspect of the right hip; the right sciatic nerve appeared enlarged and hyperintense on T2w image compared to the contralateral nerve. The right sciatic was partially entrapped by inflammatory tissue on contrast-enhanced MRI (Fig. 4a-d); STIR images revealed a small oedema area of the right femoral head (Fig. 4e).
Discussion
Hip dislocation is relatively rare in in the pediatric population, accounting for 5% of all dislocations of the hip; it is usually related to falls, motor vehicle accidents, sports and recreation, but trivial forces are involved in early childhood [1–6]. In younger children concomitant acetabular and/or femoral head fracture are occasionally observed because of ligamentous laxity, which, however, predisposes to dislocation recurrence [1, 5].
Posterior hip dislocation is more frequent than anterior dislocation [2], and results from a direct force along the femur with the hip flexed and adducted; classification of posterior hip dislocations takes associated bone fractures into account [1]:
- Grade I: Dislocation without fracture or with a minimal lesion of the acetabulum
- Grade II: Dislocation with rim fracture with congruent socket
- Grade III: Dislocation and comminution of the acetabulum rim causing instability
- Grade IV: Dislocation with fracture of the acetabular rim and floor
- Grade V: Dislocation with a fracture of the head or neck of the femur
CT and/or MRI are mandatory in case of an incomplete reduction or instability after closed reduction to detect associated lesions (such as acetabular wall fracture, interposed osteochondral fragment, labrum lesion, round ligament avulsion) which require surgical repair [2, 5, 7].
Complications of posterior hip dislocation include femoral head avascular necrosis, myositis ossificans, growth disturbance, coxa magna, neurological injury, recurrent dislocation and posttraumatic arthritis; early reduction is recommended for preventing avascular necrosis of the femoral head [1–5]. Approximately 20% of children with posterior hip dislocation experience a sciatic nerve injury, which may be related to laceration, stretching or late entrapment in heterotopic calcification; the lesions is usually consistent with neuropraxia (lesion in continuity) due to compression/stretching of the sciatic nerve, which has a favourable prognosis [3, 4, 6, 8]. Sciatic nerve palsy can also complicate close reduction of hip dislocation [8]. The peroneal division of the sciatic nerve is prone to injury more than the tibial division mainly because of a limited mobility since it is tethered proximally in the greater sciatic notch and distally in a fibrous tunnel around the knee [9]. MRI diagnosis of a stretching injury of peripheral nerves relies on morphologic continuity of nerves which appear thickened and hyperintense on T2WI [10, 11]; nevertheless detection of a tiny intra-axonal rupture is beyond MRI capability.
Differential Diagnosis List
Final Diagnosis
Sciatic nerve palsy secondary to posterior hip dislocation
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Plain film (AP view)
Computed tomography (* acetabular cavity)


Plain film after closed reduction


MRI (arrow: right sciatic nerve; curved arrow left sciatic nerve)





1. Imaging Findings
(1) X-ray Plain Film: Previously, the right femoral head was dislocated posteriorly. After closed reduction, the joint alignment appears largely restored; however, a small bony fragment is suspect near the posterior edge, indicating a possible posterior acetabular rim fracture or avulsion fracture.
(2) CT Examination: A bony fragment can be observed at the posterior edge of the right acetabulum (marked with “*”), irregular in shape, clearly demarcated from the surrounding soft tissue. After reduction, the femoral head and acetabulum are mostly aligned, but the joint space appears slightly irregular locally.
(3) MRI Examination: Abnormal signals can be observed around the area where the femoral head meets the posterior acetabular rim, potentially involving cartilage, bone, or the joint capsule. Surrounding soft tissue (including the sciatic nerve) shows thickening and high signal on T2-weighted images, suggesting neural edema or inflammatory changes due to stretching or compression. No clear signs of complete nerve rupture are seen.
2. Potential Diagnoses
Based on the history of trauma, physical examination findings, and imaging results, the following diagnoses are primarily considered:
(1) Right posterior hip dislocation with posterior rim fracture: The mechanism of injury involves direct force or axial loading to the posterior aspect of the hip, evidenced by the fractured fragments of the posterior acetabular rim on imaging.
(2) Stretch or compressive injury to the sciatic nerve: The sciatic nerve is prone to compression or stretching when the hip is dislocated posteriorly. MRI findings of neural thickening and high signal suggest edema.
(3) Other associated injuries (e.g., cartilage damage or impacted bone fragments): Vigilance is required for potential damage to the joint surface or entrapment of bone fragments that could lead to instability and long-term joint problems.
3. Final Diagnosis
Considering the patient’s age (9 years), history of trauma (knocked down while playing soccer), clinical findings (posterior dislocation of the femoral head and L4-S1 sensory/motor deficits), and imaging results (acetabular posterior rim fracture fragments and T2 high signal in the sciatic nerve region), the most likely diagnosis is:
“Right posterior hip dislocation (with posterior acetabular rim fracture) and partial sciatic nerve (L4-S1) injury.”
The nerve injury is more suggestive of nerve continuity disruption (conductive block or temporary axonal dysfunction, often referred to as a stretch-induced neuropraxia or partial nerve palsy) with generally favorable prognosis.
4. Treatment Plan and Rehabilitation
(1) Treatment Strategy:
• Maintain stable reduction: For joints that are poorly aligned or exhibit articular instability, surgical exploration and fixation of bony fragments may be necessary to prevent re-dislocation and later degenerative changes.
• Protect the sciatic nerve: Consider decongestant therapy, neurotrophic medications, and close monitoring of nerve recovery.
• Prevent femoral head necrosis: Since children’s blood supply is fragile, close follow-up is essential. If necrosis or collapse of the femoral head occurs, further treatment evaluation will be required.
(2) Rehabilitation/Exercise Prescription Recommendation (FITT-VP Principle):
• Early Stage (1–4 weeks):
- Frequency: 3–4 times per week.
- Intensity: Avoid provoking significant pain or fatigue; focus mainly on passive and active range-of-motion (ROM) exercises, taking care to protect the posterior aspect of the hip.
- Time: 15–20 minutes per session, gradually increasing.
- Type: Light lower limb support exercises, ROM training, and sciatic nerve mobilization techniques.
- Volume/Progression: Gradually increase the duration and extend the range of motion as pain and fatigue improve.
• Middle Stage (4–8 weeks):
- Emphasize joint stability and muscle strength; low-load resistance exercises (e.g., with resistance bands) under professional guidance, along with sciatic nerve mobilization.
- Gradually increase walking distance and time, using crutches or braces to offload stress on the hip.
• Late Stage (8 weeks to 3 months or beyond):
- Progress to systemic functional recovery exercises, including weight-bearing, gait training, and core muscle strengthening.
- Once the fracture has healed and joint function is satisfactory, gradually resume running, jumping, and agility exercises, with strict evaluation to prevent re-injury.
Disclaimer: The above report content is for clinical reference only and cannot replace in-person consultation or professional medical advice. In case of any doubts, it is recommended to consult with an orthopedic specialist for further discussion and follow-up.
Human Doctor Final Diagnosis
Sciatic nerve palsy secondary to posterior hip dislocation