


The patient attended the emergency room with intense pain in the right anatomical snuffbox after a fall. The X-ray was interpreted as normal and the patient discharged.
A week after the patient returned and did another X -ray where a fracture could was depicted, and CT was performed for better evaluation.
Initial X-ray:
Interpreted as normal by the resident physician but with careful attention a fracture can be depicted.
2nd X-ray:
Line of fracture can be clearly depicted in the frontal projection.
CT at the 2 visit.
Fracture of the proximal 1/3 of the right scaphoid not consolidated, aligned, persisting central non-union with cystic transformation.
No other fractures associated or complications of any kind.
No small parts alteration.
Without articular effusion.
The eight carpal bones and their corresponding ligaments can be divided into two horizontal rows with the proximal consisting of the scaphoid, lunate, and triquetrum. [2, 3]
Scaphoid fracture is the most common carpal fracture most often affecting active men [4]. The most common mechanism is hyperextension, after a fall on an outstretched hand with forced dorsifexion of the wrist [4].
They are often missed with the use of conventional radiographs alone. Initial radiographs detect at most 70% of all scaphoid fractures [1]. Anterior-posterior and lateral radiographs should be standard.
Even on the repeated radiographic exam after 10-14 days propagated by many clinicians in case of an occult fracture, a scaphoid fracture may be missed [1].
CT has an increasing role in the evaluation of patients with suspected scaphoid fractures but negative radiographs. The reported sensitivities and specificities of CT are 89%–97% and 85%– 100%, respectively [3, 5, 6]
Several fracture classification systems exist for the documentation of scaphoid fracture. Russe classification system [5] based on the orientation. Vertical oblique fractures were considered the least stable and most likely to require surgical intervention. Cooney et al [5] proposed that scaphoid fractures be considered as either nondisplaced or displaced. Herbert [6] proposed a more detailed classification scheme. Because each of these classifications emphasizes a particular aspect of the fracture, the radiologist should fully characterize the fracture and include the orientation of the fracture, displacement, and angulation.
Scaphoid non-union has been associated with the development of late arthritis of the wrist, and this pattern is commonly referred to as scaphoid non-union advanced collapse [7].
Inconspicuous radiographs in the presence of snuffbox tenderness, and wrist trauma history demand immobilization or imaging [6]. When immobilized, repeat radiographs should be done after 7 to 10 days [7]. Cystic changes and fragmentation may occur.
Any intervention may be modified based on patient hand dominance, effort, and fracture location [8]. Patient factors notwithstanding, nondisplaced stable fractures can be treated with a cast, with success of almost 95% [8]. Healing times average 8–12 weeks for the nondisplaced fracture [7, 8]. A scaphoid fracture is not considered united unless progressive loss of fracture line visibility on imaging is documented (8). In our case the orthopaedic surgeon decides to place a cast in the hand and the patient will go to rehabilitation after healing.
Take Home messages
- Scaphoid fracture is not necessarily excluded with conventional radiography
- Sequelae of scaphoid fracture are common
- Close follow-up is mandatory
Scaphoid fracture
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.




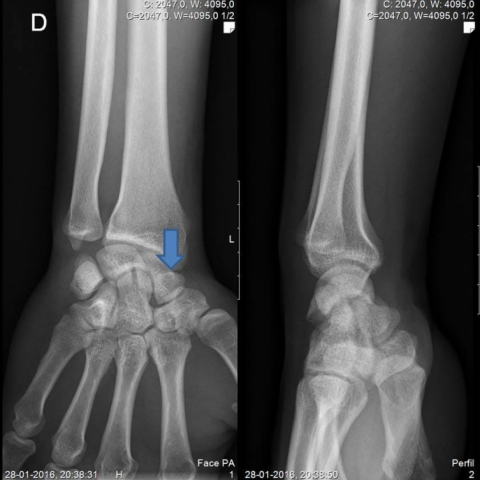

Based on the provided X-ray and CT images, there is a clear interruption of the cortical continuity in the right scaphoid region, with both distal and proximal fracture lines visibly distinguishable. During the first X-ray, the fracture line was not apparent or was poorly defined; however, in the second X-ray and subsequent CT scan, a scaphoid fracture line was definitively observed. CT reconstruction also indicates a horizontal crack in the scaphoid (in both the coronal and sagittal planes) with slight separation, though there is no significant displacement or malalignment. There is mild soft tissue swelling surrounding the site, and no obvious free fracture fragments are noted.
In summary, the imaging findings and clinical presentation most closely align with a “scaphoid fracture.” It is not uncommon for the initial X-ray to miss or fail to clearly show the fracture line in scaphoid fractures.
Taking into account the patient’s young age, trauma history (fall on an outstretched hand), anatomical location (tenderness in the anatomical snuffbox), and the clear fracture line shown on the second X-ray and CT, the most likely final diagnosis is: Right Scaphoid Fracture.
Once the cast is removed or the fracture shows a stable healing trend, a gradual rehabilitation program should be initiated to prevent joint stiffness and muscle weakness. An individualized plan following the FITT-VP principle can be implemented:
For patients with osteoporosis, long-term medication use, or compromised cardiopulmonary function, close monitoring is necessary. Progression should be gradual, with professional guidance to ensure safety when increasing exercise intensity.
Disclaimer: The above report is for reference only and does not replace an in-person consultation or professional medical advice. If you have any questions or experience any unusual symptoms, please seek prompt medical attention for an individualized treatment plan.
Scaphoid fracture