


A 45-year-old male without relevant medical casework, was referred due to pain in the posterior face of the right thigh without tumoration appearance. It became continuous with mobility affection in the territory of the sciatic nerve with impossibility for extension and knee in flexus of 45 degrees. No previous traumatism known or remembered.
A magnetic resonance study realized in his reference centre (Fig.1) demonstrated a fusiform lesion in the territory of the right sciatic nerve, within the muscles bellies of the femoral biceps and semitendinosus. Important STIR hyperintesity of the lesion and adjacent tissues with intense and homogeneous catchment of contrast by the lesion was seen.
Updating the imaging in our centre three months later (Fig.2), we demonstrated that the known lesion had well defined borders, isointensity of its signal to muscle and important reduction of associated oedema. Homogeneous contrast catchment was present but significantly less intense than in the previous study. New appearances of cartographic calcification in T2* sequence was seen. A muscular haematoma within semitendinosus muscle secondary to biopsy was also seen.
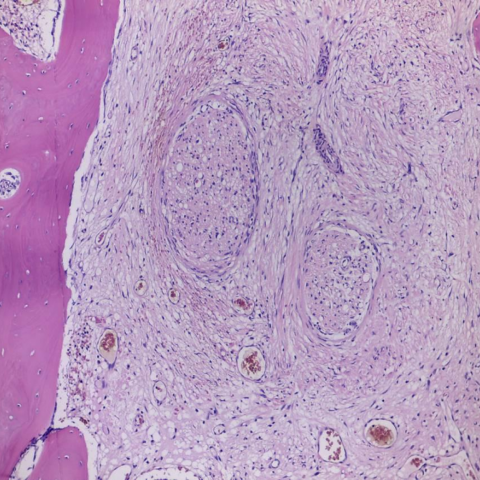
Complete exeresis of the hard-osseus lesion adherent to the sciatic nerve was performed. Histopathological examination revealed lax fibrous tissue with multiple mature osseus trabeculae (Fig. 3).
Based on the evolution of imaging findings and histology, the diagnosis of neuritis ossificans was set.
Neuritis ossificans is a very rare condition affecting peripheral nerves and is challenging to diagnose and treat [1, 2]. Due to its low prevalence, there is only sparse literature available about this pathology. Described cases affect basically the peripheral nerves of upper and lower extremities, with only one published case of cranial nerve affectation [2]. The exact aetiology is unknown but it is postulated that a previous or repeated traumatism is involved in its pathogenesis [1-3, 6].
The most frequent form of presentation is like a painful mononeuropathy and should be considered in the differential diagnosis, specially in those that appear in atypical locations for nervous compression [1]. The symptoms often present acutely with pain and paraesthesia and variable degrees of affectation of the nerve function. Palpable lesions are not always found on examination [4].
This disease shares the clinical course, anatomopathologic and imaging findings with myositis ossificans, with which it is often confused. The architecture of the lesion presents a well defined zonal differentiation with a fibroblastic centre, osteoid formation zone and external zone of ossification [1-6]. It affects a segment of a nerve and is usually confined to the epineurium [2, 5].
Diagnosis requires an elevated clinical suspicion with an accurate radiological and pathological evaluation. Athough there are no pathogmonic features, magnetic resonance is an excellent diagnostic modality showing the inflammatory reaction around the nerve [4].
In most cases in the literature, surgical treatment was chosen to prevent further neurologic deterioration [2]. However, some cases had favourable evolution with only medical treatment such as non-steroidal and steroidal anti-inflamatories [3]. Surgical excision of the tumour usually eases pain and improves nerve function, as long as the nerve can be sufficiently spared.
Our patient evolved favourably. One year after the surgical intervention, the patient had completely recovered with no neurological deficit and could be discharged.
In conclusion, neuritis ossificans is a very rare pathology but potentially under acknowledged [1]. It must be kept in mind in the differential diagnosis of painful mononeuropathies in order to set a correct diagnosis [1]. Magnetic resonance is an excellent imaging modality due to its good tissular definition. Surgical treatment is healing but nervous sparing can often be difficult [5, 6].
Neuritis ossificans
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.














Based on the provided MRI data, a localized lesion can be observed in the right posterior thigh region, around the sciatic nerve. The lesion is relatively well-demarcated from the surrounding soft tissues. On T1-weighted images, the lesion’s signal mostly resembles adjacent soft tissue. On T2-weighted and fat-suppressed sequences, there is evidence of mixed abnormal signals, with areas suggesting inflammatory reaction or edema. Inside the lesion, ring-shaped or patchy high/low signal areas indicating potential ossification or calcification can be observed, suggesting ossified tissue. Overall, the lesion is located around or within a peripheral nerve (suspected sciatic nerve), and its imaging characteristics differ from common schwannomas or typical tendon/muscle lesions. Further correlation with clinical history and pathological analysis is required.
Considering a 45-year-old male patient with persistent right posterior thigh pain, accompanied by sciatic nerve-related functional impairment, without a clear history of trauma, and MRI revealing an abnormal ossifying or calcifying lesion around the nerve, along with intraoperative findings of a nerve-surrounding lesion pathologically confirmed to be an ossifying lesion, the most likely diagnosis is:
Neuritis Ossificans.
This condition is rare and often only recognized when local nerve pain, sensory deficits, and ossification or calcification features are noted. Definitive diagnosis typically requires surgical intervention and pathological confirmation.
During rehabilitation, an individualized exercise program should be developed based on the patient’s condition, surgical extent, and degree of nerve involvement. Below is an example recommendation:
Throughout rehabilitation, closely monitor pain, swelling, or changes in nerve symptoms. Seek medical attention promptly if unusual or worsening symptoms occur. In patients with additional comorbidities (e.g., osteoporosis or impaired cardiopulmonary function), exercise intensity and modalities should be chosen with greater caution to ensure safety.
This report offers a medical reference based on existing history and imaging data and does not replace an in-person consultation or professional medical advice. Patients should attend regular follow-ups and develop or modify treatment and rehabilitation plans under the guidance of qualified healthcare professionals.
Neuritis ossificans