Dysbaric osteonecrosis of the humerus



Clinical History
A 42-year-old recreational diver presented with progressive pain at the right shoulder two hours following diving. History of recent trauma was denied.
Imaging Findings
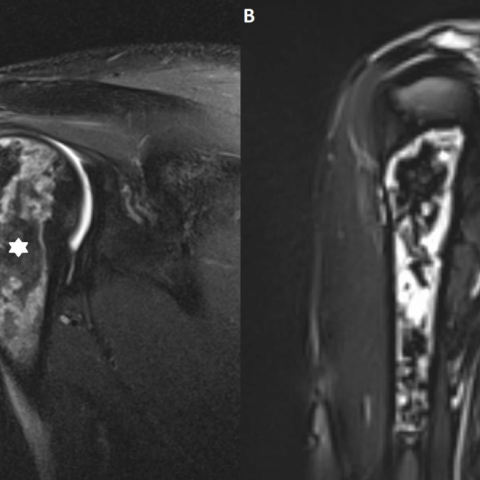
Plain radiographs revealed no abnormalities (Fig. 1). Magnetic resonance (MR) arthrography of the right shoulder 4 weeks after the onset of pain was requested in order to exclude rotator cuff disease and bone marrow disease. MR revealed an irregular aspect of the articular side of the supraspinatus tendon (Fig. 2A). MRI also showed an extensive area of abnormal bone marrow within the proximal diaphysis of the humerus, with extension into the humeral head (Fig. 2B, Fig. 3A and B). Coronal T1-weighted images (T1-WI) of the right humerus (Fig. 3) showed a peripheral rim of low signal intensity (SI) surrounding a central zone similar to fat. On coronal fat suppressed T2-WI (Fig. 4A and B), the peripheral borders were strongly hyperintense. Coronal T2-WI (Fig. 5) showed a double-line sign consisting of a hyperintense rim centrally surrounded by a hypointense rim peripherally. There was no soft tissue involvement.
Discussion
Based on the imaging findings and clinical history of the patient, diagnosis of dysbaric osteonecrosis (DON) was made.
DON is a manifestation of decompression illness (DCI). Other commonly used terms are Caisson disease, the bends, and diver’s disease. DON results from nitrogen gas bubble formation following an excessive drop in atmospheric pressure, in divers during rapid ascent, or in pilots after urgent increase of altitude [1].
DON usually affects fatty-marrow containing long bones, particularly the proximal third of the humerus and tibia and distal third of the femur [2]. This can be explained by the fact that nitrogen is more soluble in fat [3]. Obstruction of intramedullary sinusoids by gas bubbles results in blood stasis, ischemia and bone necrosis causing joint pain (acute type I of DCI). Furthermore intramedullary pressure changes may aggravate venous stasis [3]. In type II of DCI, neurologic, pulmonary and circulatory symptoms predominate.
Clinical information is crucial to make a final diagnosis as imaging of DON is not different from other causes of bone infarcts.
Plain radiography lacks sensitivity for early detection of DON. Typical radiographic findings include increased bone density, subarticular crescent sign and geographically delineated bone infarcts with sclerotic borders. These findings are only visible after weeks or months and represent late, irreversible lesions.
MRI is the preferred technique for early diagnosis. Devascularized areas tend to form well-demarcated lesions with a characteristic serpiginous geographic pattern [4]. Typically, a peripheral double-line sign is seen on T2-WI, consisting of an inner rim of high SI surrounded by an outer rim of low SI. It was initially explained by an inflammatory response around the central ischemic core resulting in a hyperintense inner zone of hyperemic granulation tissue and a hypointense outer rim of reactive sclerosis [5]. Alternatively, the double line sign may be caused by a chemical shift artefact, explaining reversal of these alternating hypointense and hyperintense rims. The central part of osteonecrotic bone marrow may have a variable SI. Most often, due to mummification of dead fatty marrow, the SI resembles fat on all pulse sequences, although edematous or fibrotic changes may occur [4].
Scintigraphy is sensitive to detect early ischemic bone marrow changes, its low specificity hampers its usefulness in diagnosing DON.
The prognosis depends upon early diagnosis and prompt treatment, consisting of hyperbaric oxygen therapy in a recompression chamber. This has been applied twice in our patient with complete resolution of pain within 1 week following treatment.
Differential Diagnosis List
Final Diagnosis
Dysbaric osteonecrosis of humerus
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Radiograph

MR arthrography, fs T1-WI

MR arthrography, fs T2-WI
MR arthrography, T2-WI

Coronal T1-WI MR Images

Imaging Findings
1. X-ray Plain Film: The anteroposterior view of the right shoulder joint shows mildly abnormal bone density in the proximal humerus. No obvious fracture line is visible, but there is slight blurring and density changes in the local area.
2. MRI: A well-defined abnormal signal is noted in the medullary cavity of the proximal humerus. On T2-weighted images, the “double-line sign” is observed (i.e., high signal on the inner rim and low signal on the outer rim), and loss or significant reduction of fat signal in some areas suggests coexisting bone marrow necrosis and repair. These findings are typical of early ischemic osteonecrosis.
Possible Diagnoses
Based on the patient’s history of diving and the ischemic changes seen on imaging, the following differential diagnoses can be considered:
1. Dysbaric Osteonecrosis: The patient’s recent diving history, rapid onset, characteristic shoulder pain, and typical imaging findings of intramedullary necrosis strongly support this diagnosis.
2. Osteonecrosis of Other Etiologies (e.g., Steroid-Induced): Common in patients with long-term use of corticosteroids or other vascular compromise, but there is no relevant medical history in this case.
3. Bone Infarction: Seen in conditions such as sickle cell disease or thrombotic disorders, usually with different clinical history and imaging characteristics. The clinical background here does not fully match.
4. Infectious or Neoplastic Lesions: Chronic osteomyelitis or malignancy should be ruled out based on clinical findings, laboratory tests, or pathology. However, current evidence does not directly point to these pathologies.
Final Diagnosis
Taking into account the patient’s age (42-year-old male), recent history of diving, timing of pain onset (approximately 2 hours after diving), and imaging findings (double-line sign, localized ischemic changes), the most likely diagnosis is: Dysbaric Osteonecrosis.
Treatment Plan and Rehabilitation Program
1. Treatment Strategy:
- Hyperbaric Oxygen Therapy: Early and timely hyperbaric oxygen and recompression treatment can help alleviate pain and slow or delay further progression of bone necrosis.
- Symptomatic Management: Use of NSAIDs or analgesics as necessary to relieve acute pain.
- Monitoring and Follow-up: Regular MRI or other imaging studies to assess the extent of osteonecrosis and stability of bone structure.
- Surgical Intervention: If the condition progresses or if joint collapse and severe pain affect quality of life, options such as joint surface replacement or other surgical procedures may be considered.
2. Rehabilitation and Exercise Prescription:
- Principles: Gradual progression with individualized design, avoiding excessive stress or high-impact activities; emphasize restoring and protecting shoulder joint function and adjacent muscle groups.
- FITT-VP Recommendations:
• Frequency: 3–5 times a week, depending on the degree of symptom relief.
• Intensity: Start with low intensity with no or minimal load, e.g., active range-of-motion exercises using a sling. Gradually progress to light resistance training.
• Time: 15–30 minutes per session, adjusted according to pain and fatigue levels.
• Type: Range-of-motion exercises (active or passive), shoulder girdle strengthening (light resistance bands or dumbbells), and water-based exercises (to minimize joint stress).
• Progression and Volume: Increase load or extend training duration as pain resolves and strength improves, while closely monitoring joint response.
- Precautions:
• Avoid diving or other high-risk situations, especially during the acute recovery phase. Follow professional recommendations.
• If significant pain, swelling, or functional limitation occurs, stop training and seek medical evaluation.
• Emphasize training for flexibility and stability of the shoulder joint and surrounding muscles to prevent secondary adhesive capsulitis or contractures.
• If the patient has other chronic diseases or poor overall fitness, collaborate with rehabilitation and cardiology professionals to tailor the program.
Disclaimer: This report is based solely on the provided medical history and imaging data for reference purposes and cannot replace an in-person consultation or a professional medical diagnosis. If you have any questions or if symptoms worsen, please seek medical attention promptly.
Human Doctor Final Diagnosis
Dysbaric osteonecrosis of humerus