Pott's spine with psoas abscess



Clinical History
A 50-year-old female patient presented with low back pain for 3 months. She had experienced difficulty in standing up from sitting position for 15 days. She had associated complains of low-grade fever and weight loss for 3-4 months. The patient was referred for MRI of the lumbosacral spine.
Imaging Findings
CT shows end plate irregularity and sclerosis of L3 and L4 vertebral bodies with decreased height of intervening L3-L4 intervertebral disc (Fig. 1, 2).
MRI shows irregularity and destruction of L3-L4 end plates and intervertebral disc with well-defined collection in the prevertebral and bilateral paravartebral regions (Fig. 5, 6) which appears hypointense on T1W (Fig. 3, 5) and hyperintense on T2W (Fig. 4, 6). The collection is seen extending in the left psoas muscle leading to psoas abscess (Fig. 6). A small epidural collection is seen at the level of L3 and L4 vertebrae which is causing compression over the spinal cord (Fig. 4b).
Discussion
Musculoskeletal involvement of TB is estimated in 1–13 % of patients and spine is affected in more than 50% of cases. “Pott’s Disease” (tuberculous spondylitis) represents the most common form of extrapulmonary TB. The thoracic segments are the preferred sites, followed by the lumbar levels. Pott's spine involves two contiguous vertebral bodies with the intervening disk, but multilevel extension (three or more vertebrae) characterizes the disease[1].The paradiscal, central, anterior subligamentous, and neural arch are the common vertebral lesions. In Pott's spine, the onset of symptoms is usually insidious and progression is slow.
In the paradiscal type, the earliest features are narrowing of the joint space and indistinct paradiscal margin of vertebral bodies. With further progression, anterior wedging or collapse occurs, resulting in varying degree of kyphosis.
In the anterior type of the lesion, the collection of tuberculous granulation tissue and necrotic material leads to formation of paravertebral abscess which is visible on plain radiographs as a fusiform radiodense shadow called the bird nest appearance. Long standing abscesses may produce concave erosions around the anterior margins of the vertebral bodies producing a scalloped appearance called the aneurysmal phenomenon (gouge defect).
The central type of the lesion presents as destruction, ballooning of vertebral bodies, and concentric collapse.
In the neural arch type of the lesion, there is involvement of the posterior arches (spinous process, lamina, pedicle, and transverse process as well as lateral masses of the atlas), pedicular or laminar destruction, erosion of the adjacent ribs in the thoracic region or posterior cortex of the vertebral body with relative sparing of the intervertebral discs, and a large paraspinal mass.
The pattern of bone destruction (fragmentary, osteolytic, sclerotic, and subperiosteal) can be seen well on CT. The presence of calcification within the abscess is virtually diagnostic of spinal TB [2]. Most cases of the active disease have paraspinal (subligamentous, psoas, epidural) soft tissue masses [3]. MRI features of Pott's spine appear hypointense on T1W and hyperintense on T2W sequences with heterogeneous enhancement of the vertebral body. STIR sequences are helpful in differentiating fluid from fatty components in non-contrast sequences. Administration of Gd-DTPA is useful to assess the extent of soft tissue mass. Kyphosis and cord compressions are the most common complications [2].
Treatment with antituberculous medications with surgical debridement and reconstruction of spinal stability are the key aspects [4].
It is often difficult to differentiate between tuberculous and pyogenic spondylitis, both clinically and on images. When infection is suspected, a history of chronicity and insidious progression is suggestive of tuberculous spondylitis [5].
Differential Diagnosis List
Final Diagnosis
Pott's spine with psoas abscess
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
CT Bone window


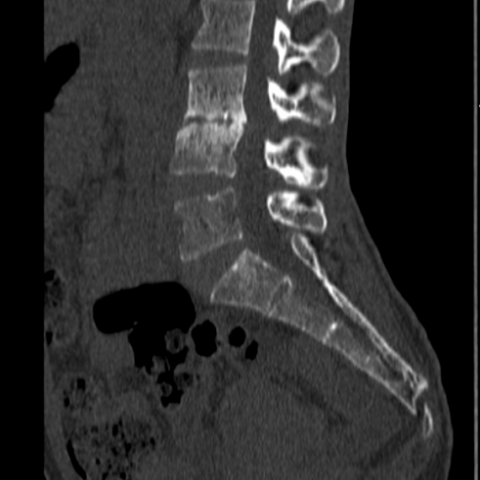
CT Soft tissue window


MRI LS Spine Sagittal


MRI LS Spine Axial T2W image


MRI LS Spine Axial TIW image


MRI LS Spine Coronal


Medical Imaging Analysis Report
I. Radiological Findings
Based on the provided lumbar spine CT and MRI images, the following main features are observed:
- There is bony destruction and collapse in parts of the lumbar vertebral bodies (predominantly in the lower lumbar segments), showing irregular vertebral margins.
- Paravertebral soft tissue swelling or a mass-like shadow is visible, suggesting a possible paravertebral abscess or granulation tissue (appearing as lower or slightly lower density than soft tissue on CT, and presenting as low T1 signal and high T2 signal on MRI).
- Some vertebral body margins appear indistinct, and the intervertebral disc may be involved, showing narrowed intervertebral space (particularly evident on CT).
- On MRI, the involved vertebral bodies show decreased signal on T1W sequences and high signal on T2W sequences. After contrast administration, the lesions show heterogeneous enhancement. On STIR sequences, the soft tissue and vertebral lesions demonstrate increased signal intensity.
- An abnormal signal shadow in the psoas region or paravertebral soft tissue further suggests the formation of an abscess.
II. Potential Diagnoses
Considering the patient’s chronic lower back pain, low-grade fever, weight loss, and the imaging characteristics noted above, the following diagnoses should be considered:
-
1. Tuberculous Spondylitis (Pott’s Disease):
This condition often presents as a chronic or subacute process, commonly involving two adjacent vertebrae and the intervertebral disc. It may lead to vertebral collapse and paravertebral abscess formation. When accompanied by low-grade fever, weight loss, and back pain, a high level of suspicion is warranted. -
2. Pyogenic (Bacterial) Spondylitis:
Commonly caused by typical bacteria (e.g., Staphylococcus aureus). Its imaging findings can be similar to those of tuberculosis, including vertebral destruction and disc involvement, though the course is usually more acute, with more severe local pain and notably higher systemic inflammatory responses. If tuberculosis is unlikely or the course is rapidly progressing, this diagnosis should be considered. -
3. Other Causes of Vertebral Lesions:
Such as metastatic tumors, fungal infections, or brucellar spondylitis, which can also show bone destruction and soft tissue masses. These conditions often have specific medical histories or distinct laboratory findings and require comprehensive evaluation.
III. Final Diagnosis
Based on the patient’s:
- Age and long-term history of low back pain;
- Persistent low-grade fever, weight loss, and other systemic symptoms;
- Imaging findings (vertebral destruction, disc involvement, paravertebral/psoas abscess-like changes, heterogeneous enhancement);
The most likely diagnosis is Tuberculous Spondylitis (Pott’s Disease). For definitive confirmation, it is recommended to perform further laboratory tests (such as T-SPOT.TB, tuberculin skin test, serological evaluations) or conduct a biopsy of the lesion to confirm the pathogenic organism if necessary.
IV. Treatment Plan and Rehabilitation
1. Overview of Treatment Strategy
- Medication: Antituberculous therapy is the first choice, typically involving a standard combination of antituberculous drugs for at least 6–9 months. The specific regimen may vary according to local guidelines or specialist advice.
- Surgical Intervention: For severe vertebral destruction, significant spinal cord or nerve compression, ineffective conservative treatment, or the development of marked deformities, surgical decompression, lesion debridement, and spinal structural reconstruction (e.g., bone grafting and fusion) may be considered.
- Supportive Care: Includes adequate nutrition, maintenance of a healthy physical and immunological status, and the use of a spinal brace when necessary to stabilize the spine and alleviate pain.
2. Rehabilitation Training Recommendations (FITT-VP Principle)
Rehabilitation should be conducted under the guidance of healthcare professionals and physical therapists, starting from low intensity and progressing gradually:
- Frequency (F): According to patient tolerance, 3–5 times per week; early-stage sessions may be reduced to 2–3 times per week as needed.
- Intensity (I): Begin with low intensity, ensuring no pain or only mild pain. A back brace may be used for support if necessary.
- Time (T): 20–30 minutes per session, which can be divided into segments. Duration can be gradually extended as endurance improves.
- Type (T):
- Early Stage: Focus on respiratory function exercises and maintaining lower limb muscle strength (e.g., straight leg raises, ankle pump exercises), avoiding excessive spinal loading.
- Intermediate Stage: Once pain relief and stability are achieved, introduce gentle stretching, core stabilization (e.g., core activation on a firm bed), and light walking or swimming to enhance cardiopulmonary endurance.
- Later Stage: Depending on bone healing and inflammation control, progressively increase resistance training with elastic bands or light weights to strengthen paraspinal muscles.
- Progression (P): Gradually increase the training load based on follow-up imaging, pain assessments, and overall physical function. Carefully monitor spinal stability and any neurological symptoms.
Throughout this process, special attention should be paid to bone fragility and overall physical condition. Proper technique and safety must be ensured.
Disclaimer
This report provides a reference analysis based on the patient’s imaging and basic clinical information. It is not a substitute for an in-person clinical diagnosis or professional medical advice. For specific treatment decisions, please follow the guidance of a specialist and the results of further examinations.
Human Doctor Final Diagnosis
Pott's spine with psoas abscess