Periosteal plexiform neurofibroma of the femur



Clinical History
A 37-year-old man consulted for discomfort with months of evolution in the posterior aspect of the left knee, especially on flexion. In addition, clinical exam revealed a doubtful positive meniscal manoeuvre. The patient has neurofibromatosis type 1 (NF1). Knee radiographs were requested.
Imaging Findings
Radiographs showed sclerosis and scalloping of the posterior cortex of the femur (Figures 1a and 1b).
MRI demonstrated a soft tissue and polylobulated mass located next to the posterior aspect of the femur, with intermediate to low signal intensity on T1WI (Figures 2a, 2b and 2c), hyperintense and heterogeneous on PD-FSE-WI (Figures 3a, 3b and 3c) and intense enhancement after GdDPTA contrast administration (Figures 4a, 4b and 4c). DWI demonstrated an intermediate value on ADC (1.67x10^-3 mm2/s) (Figures 5a and 5b).
The lesion conditioned polylobulated scalloping of the femur, without cortical breakthrough or bone marrow oedema, raising the doubt of its origin, whether it was dependent on the periosteum or the adjacent soft tissues.
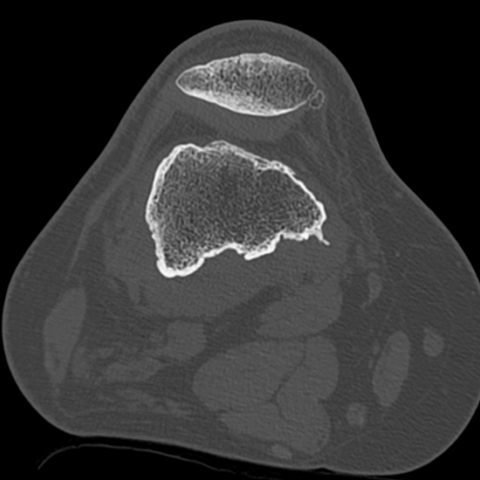
CT scan was performed to assess bone involvement, showing thickening of the cortex with associated sclerosis, confirming the chronic behaviour of the lesion (Figures 6a and 6b).
Imaging findings together with the history of NF1 allowed us the diagnosis of a periosteal plexiform neurofibroma (PPN) of the femur. As the lesion had benign behaviour and it was clinically stable, conservative management with follow-up by MRI was decided.
Discussion
Background
Plexiform neurofibroma (PN) is one of the types of peripheral nerve sheath tumour (PNST). It is a specific tumour for NF1. Although it is a benign lesion, it may become malignant in 10% of cases [1–4].
The periosteum is a highly innervated tissue, so it is a target organ for PN. However, there are few cases of periosteal origin of PN described in the literature, and most of the cases are smaller, making our case interesting [5,6].
Clinical Perspective
The clinical manifestations are varied, ranging from asymptomatic patients to others with severe functional deficits. It is also described as presenting pain due to bleeding [2–6].
Imaging Perspective
MRI is considered the imaging method of choice to study PN [2–4]. MRI for PPN shows the typical characteristics of a PN: a soft tissue lesion of polylobulated morphology, with intermediate-low signal in T1WI, hyperintense in T2WI and with an intense enhancement after contrast administration [2–6]. Nevertheless, there are some particularities, such as its location (closely related to the periosteum) and the reactive thickening of the adjacent bone cortex in a lobulated and smooth way, as we demonstrated in our case [5,6].
Its imaging features may be similar to other PNSTs, and therefore, it is essential to know the patient’s clinical context to make a confident diagnosis by imaging [2,5]. Due to its location, the differential diagnosis should also include benign cortical bone lesions such as non-ossifying fibroma, juxtacortical chondroid tumours, and even surface osteosarcoma [7,8].
Follow-up has been accepted as a good treatment alternative unless clinical symptoms are predominant. Imaging features changes may suggest malignant degeneration, such as invasion of the cortex, necrosis or poorly differentiated borders [1,9–11]. However, sometimes, it can be difficult to differentiate a benign finding from malignant degeneration on standard MRI. In these cases, lower ADC values have been proven to be more associated with malignant degeneration than intermediate values. For this reason, ADC values determined by DWI combined with T1WI and T2WI, and also dynamic contrast-enhanced (DCE) sequences, have great sensitivity and specificity to differentiate malignant degeneration from a benign PN [1,9–11]. FDG-PET is useful in this situation too, but its cut-off value is lower than DWI and DCE, showing up to a 5% false positive rate in patients with PN [1,9–12].
Biopsy is the true gold standard. Nevertheless, given the confidence of MRI in typical cases, it is usually relegated to atypical cases or those with suspected malignant degeneration [1].
Take Home Message / Teaching Points
- Although the periosteum is a target organ for PN, it is an uncommon location.
- MRI is the imaging method of choice for diagnosis.
- Clinical context is essential to diagnose PN by imaging.
All patient data have been completely anonymised throughout the entire manuscript and related files.
Differential Diagnosis List
Final Diagnosis
Periosteal plexiform neurofibroma
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
X-ray of the knee


T1WI (MRI)



PD WI (MRI)



T1WI + GdDPTA (MRI)



DWI with the highest coefficient b and ADC map (MRI)


CT scan

Medical Imaging Analysis Report
I. Imaging Findings
1. From the anteroposterior and lateral X-ray views of the knee joint, the left knee joint structure is essentially aligned, with no obvious destructive lesions on the articular surface. However, a slight contour elevation is visible in the distal femur near the posterior soft tissue region. No clear cortical erosion is noted, and there may be mild reactive periosteal thickening or linear changes.
2. MRI in the axial, sagittal, and coronal planes shows a lobulated soft tissue mass in the distal femur posterior area near the articular surface. On T1-weighted images, the lesion mainly appears isointense or slightly hypointense, while on T2-weighted images, it shows relatively high signal. Areas of enhancement can be seen in distinctly defined regions, and the lesion tightly abuts the posterior femoral periosteum. Smooth cortical thickening is observed locally, with no clear signs of invasive destruction.
3. On diffusion-weighted imaging (DWI) and ADC maps, the lesion shows a certain degree of restricted diffusion. Contrast-enhanced scans demonstrate pronounced enhancement, suggesting abundant vascular or cellular components.
4. The adjacent articular cartilage and joint space are largely preserved. Posterior soft tissue shows a mass effect, potentially closely related to the joint capsule and popliteal structures. No overt signs of bone or cartilage destruction are observed.
II. Potential Diagnoses
Based on the patient's past medical history of Neurofibromatosis Type 1 (NF1) and the imaging findings, the following should be considered:
- Plexiform Neurofibroma (PN): Commonly seen in NF1 patients. In this case, the lesion presents a lobulated pattern, T2 hyperintensity, and is closely attached to the periosteum, with localized smooth cortical thickening—matching the typical imaging features of plexiform neurofibroma.
- Other Peripheral Nerve Sheath Tumors (e.g., schwannoma or conventional neurofibroma): Similar to PN, but plexiform neurofibroma is more distinctive, especially in the context of NF1.
- Surface Bone Tumors (e.g., osteochondroma or periosteal sarcoma): These may present as surface bone lesions, but often involve bony destruction or prominent periosteal reactions, and do not fully align with the soft tissue density or signal seen in this case.
- Soft Tissue Tumors (e.g., lipoma, hemangioma): While they can appear as local soft tissue masses, T2 hyperintensity, marked enhancement, and smooth cortical thickening are more suggestive of a neurogenic tumor.
III. Final Diagnosis
In summary, given the patient’s NF1 background, the multilobulated appearance of the lesion, its close proximity to the periosteum with localized smooth cortical thickening, and its characteristic soft tissue signals on MRI, the most likely diagnosis is:
Plexiform Neurofibroma
If malignancy is suspected or the diagnosis remains uncertain, further MRI functional imaging (DCE, DWI), PET-CT, or biopsy may be considered to clarify the nature of the lesion.
IV. Treatment Plan and Rehabilitation Program
1. Treatment Plan:
(1) Follow-up Observation: If the lesion is asymptomatic and remains stable on imaging, periodic check-ups (MRI or ultrasound) can be performed to monitor changes in size. Further intervention should be considered if there is rapid enlargement, persistent pain, or suspicion of malignant transformation (including bone destruction, unclear margins, necrotic areas, etc.).
(2) Surgical Treatment: If there are significant symptoms affecting mobility or a strong suspicion of malignant change, surgical resection can be considered. For plexiform neurofibroma, complete resection of the lesion with preservation of key neurovascular structures should be ensured.
(3) Adjuvant Therapy: In cases of malignant transformation or unclear margins, postoperative radiotherapy or chemotherapy may be considered. However, most benign lesions, if fully resected, typically do not require routine radiotherapy or chemotherapy.
2. Rehabilitation/Exercise Prescription (Based on FITT-VP Principles):
(1) Early Stage (Conservative Functional Phase):
- Frequency: 2-3 times per week, avoiding excessive fatigue and deep knee flexion with heavy loading.
- Intensity: Low-intensity lower limb strengthening exercises and simple active movements, either non-weight-bearing or assisted by light resistance bands.
- Time: 15-20 minutes per session. “Little but frequent,” increasing gradually based on patient tolerance.
- Type: Exercises such as seated knee extensions, straight-leg raises, ankle pumps, or other joint range-of-motion activities.
- Progression: As the condition stabilizes or slightly improves, increase the frequency or resistance gradually.
- Frequency: 3-4 times per week, increasing as tolerated.
- Intensity: Low to moderate weight-bearing (e.g., light-resistance static squats, resisted exercises with bands), closely monitoring pain levels.
- Time: 20-30 minutes per session, divided into multiple sets to avoid continuous strain.
- Type: Once knee strength and proprioception are stable, introduce closed-chain movements (e.g., seated leg press, partial squats), avoiding excessive angles, high speed, or impact.
- Progression: Gradually increase training difficulty and duration based on joint stability and pain levels, carefully avoiding exacerbation of any lesion-related irritation.
- Frequency: 3-5 times per week, focusing on functional exercises.
- Intensity: Moderate intensity, incorporating daily activities such as stair climbing, light jogging, or single-leg balance exercises.
- Time: Approximately 30 minutes per session, adjusted to individual needs.
- Type: Diverse training, including neuromuscular coordination, balance board work, and core stability exercises.
- Progression: Carefully monitor any changes in symptoms. If there is increased pain, growth of the lesion, or other discomfort, training should be stopped, and medical follow-up is advised.
Disclaimer: This report is for medical reference only and does not replace in-person consultations or professional medical advice. If you have any concerns or worsening symptoms, please visit a regular medical institution for evaluation.
Human Doctor Final Diagnosis
Periosteal plexiform neurofibroma