


56-year-old male patient presented with a growing subcutaneous tumour at his inner thigh on the right side. He experienced no pain. At the time of the ultrasound examination, it measured 5x5x8 cm. A pre-operative MRI scan was performed. It was diagnosed histologically as a leiomyosarcoma of the greater saphenous vein.
Ultrasound showed an irregularly vascularised and echo-poor tumour in close contact with the greater saphenous vein.
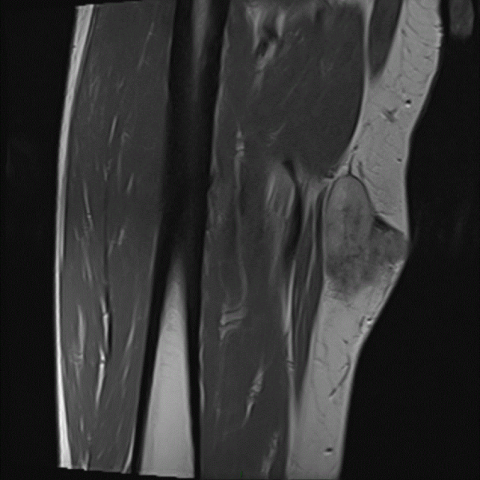
MR showed a heterogeneous hypointense process on T1 sequence before contrast with inhomogeneous contrast enhancement. In TIRM sequence the process was inhomogeneous, predominantly hyperintense.
The tumour seems (partly) to grow endovascularly in the greater saphenous vein (Fig 3a-c).
Pre-operative Positron emission tomography–computed tomography (PET-CT) showed a PET positive tumour, but no sign of metastases.
Leiomyosarcoma (LMS) in general is a rare type of malignant tumour of smooth muscle tissue, accounting for only 6 % of all soft tissue malignant tumours [1]. Only 2 % of LMS originate from major vessels and most occur in the inferior vena cava [1, 2, 3]. A review from 2016 concluded that only ~1/1.000.000 malignant tumours is LMS of the greater saphenous vein (GSV). The same review stated that only 38 cases has been reported in the literature [1].
The clinical presentation of LMS of the GSV is typically a growing mass. It can be painless, give pain on movement, or present with symptoms such as oedema and venous thrombosis. The mean age in the literature is 55-61 years [1]. The tumour arises intramurally from the tunica media of the vein. The tumour tends to develop in extra-vascular direction, but also, tends to develop intraluminal in GSV, as in this case.
Ultrasound is the primary examination of soft tissue tumours, MR comes second because it provides superior soft-tissue contrast resolution. The role of PET-CT is to determine whether the lesion is malignant and whether there are metastases. A combination of local MR, to rule out local relapse, and CT thorax and abdomen is used for follow-up.
The treatment is surgery, resection with a wide margin of 2-3 cm. There are no studies regarding adjuvant radiation and chemotherapy. At the time of diagnosis, 10 % of patients with LMS of the GSV have metastasis. The main site of metastatic disease is the lungs. Survival rate of 80-90 % after surgery is reported [1]. The patient in this case showed no sign of local relapse (MR) or metastasis on CT scan 6 month after surgery.
Leiomyosarcoma of greater saphenous vein.
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.







Based on multi-modal imaging (ultrasound, MRI, PET-CT), the following observations are noted:
• The lesion is located on the medial side of the right thigh, clinically adjacent to the course of the great saphenous vein.
• Ultrasound reveals a well-defined soft tissue mass measuring approximately 5 × 5 × 8 cm. Color Doppler shows abundant blood flow signals around and within the lesion.
• On MRI (transverse and sagittal planes), the tumor appears as a well-demarcated solid nodule with intermediate or slightly low signal intensity on T1-weighted images (T1WI), relatively high signal on T2-weighted images (T2WI), and exhibits marked enhancement. Part of the tumor seems connected to the vascular channel and displays both intraluminal and extraluminal growth.
• PET-CT shows significantly increased metabolic activity in the mass, suggesting a high possibility of malignancy.
• No obvious infiltration or destruction of the surrounding muscle structures is observed, and there are currently no notable signs of bone involvement.
Based on the clinical presentation (a painless, progressively enlarging soft tissue tumor) and the imaging characteristics (solid mass, rich vascular supply, and high metabolic activity), the differential diagnoses may include:
Combined with pathological examination results, the confirmed diagnosis is: Leiomyosarcoma of the greater saphenous vein.
This diagnosis is based on:
• Clinical: Middle-aged to older patient with a progressively enlarging, painless mass.
• Imaging: High metabolic activity, close relationship to the vessel’s course with both intraluminal and extraluminal growth.
• Pathology: Histological evidence of malignant proliferation originating from the smooth muscle cells of the venous wall.
• Surgical Resection: The primary treatment is wide surgical excision with a 2–3 cm margin to reduce local recurrence risk.
• Adjuvant Therapy: Currently, there is no strong evidence to support that routine chemotherapy or radiotherapy significantly improves survival for leiomyosarcoma of the great saphenous vein. However, in cases with a higher tumor stage or specific pathological subtypes, individualized consideration for radiotherapy or chemotherapy may be warranted.
• Follow-up: Postoperative imaging assessments (MRI or CT) are recommended at regular intervals (typically every 3–6 months) to monitor local recurrence. Chest CT should be performed to rule out pulmonary metastases. A multidisciplinary team (vascular surgery, oncology, radiology, etc.) should be involved for comprehensive management.
(1) Early Postoperative Phase:
• Protect the affected limb properly; avoid heavy load in flexion/extension movements.
• Perform mild muscle strengthening exercises, such as isometric quadriceps contractions, gradually promoting blood circulation in the lower limb.
• Maintain good wound hygiene and ensure proper incision healing.
(2) Progressive Exercise Training (FITT-VP Principle):
• Frequency: 3–5 times per week.
• Intensity: Start with low intensity (RPE 9–11), monitoring local reactions and overall tolerance. If no significant pain or swelling occurs, gradually progress to moderate intensity (RPE 12–13).
• Time: 20–30 minutes per session, beginning with continuous walking, light cycling, or water-based activities.
• Type: Emphasize low-impact exercises (e.g., cycling, swimming, seated strength training). Avoid excessive weight-bearing and vigorous twisting.
• Volume & Progression: If symptoms remain stable, increase exercise intensity or duration by 5–10 minutes every 2–4 weeks.
(3) Individual Considerations:
• Given the vascular-related surgery and recent incision, pay special attention to local swelling, wound healing, and vascular patency.
• If there is increased wound pain, redness, fluid discharge, or limb dysfunction, seek medical attention promptly.
• For patients with other chronic conditions (e.g., hypertension, poor cardiopulmonary function), exercise adjustments should be made progressively under medical and rehabilitation specialist guidance.
Disclaimer:
This report is based on the available images and basic clinical information, intended to provide reference opinions only. It does not replace in-person consultation or professional medical advice. Patients should consult their physician for any new symptoms or concerns, and further examination or treatment may be necessary.
Leiomyosarcoma of greater saphenous vein.