Atypical multiple myeloma



Clinical History
A 40-year-old female patient presented with diplopia and headache.
Laboratory investigations revealed
Hb : 9 g/dL
S. Calcium level: 15 mg/dL (borderline high).
Imaging Findings
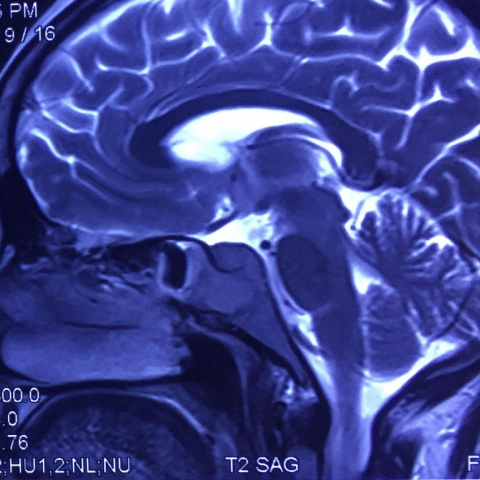
MRI brain:
Altered signal intensity lesion involving the anterior aspect of clivus extending to the bilateral parasellar region involving the both cavernous sinuses.
It appears isointense on T1W and hypointense on T2W.
Post-contrast study revealed homogeneous enhancement of the lesion.
Similar characteristic enhancing soft tissue lesions were seen involving the rami of the mandible on either side.
PET scan:
Multiple hypermetabolic lesions involving the axial and appendicular skeleton (MAX SUV: 18).
CT scan guided tru-cut biopsy:
From left para-vertebral soft tissue at dorsal vertebra.
Sent for histopathology examinations.
Discussion
Multiple myeloma is most common primary osseous malignancy of the older age group. The most common affected age group is 40 -80 years [1].
It is a disorder of plasma B cells associated with bone marrow infiltration and overproduction of monoclonal immunoglobulins.
The common presentation of the disease is generalised weakness, bone pain, pathological fracture or signs of neural compression.
The primary blood investigations include complete blood count, which demonstrates anaemia.
The further investigations are done with electrophoresis, which demonstrates increase in monoclonal immunoglobulin (M protein).
Radiological investigations are suggested for staging and prognosis.
Classical findings on X-ray show generalised osteoporosis with multiple well-defined punched-out lytic lesions without rim of sclerosis in the axial and appendicular skeleton. However, in 10-20 % skeletal survey does not reveal abnormal findings [2] and it is difficult to differentiate from the osteoporosis of the other cause like age-related, steroid-induced or alcohol intake-related. So in modern era the use of cross-sectional imaging with CT scan, MRI and PET-CT is increasing for the staging purpose or to evaluate any complication.
CT findings in multiple myeloma included osteoporosis with lytic lesions with or without the soft tissue component. CT is superior for detecting the risk of fracture. It is also useful in guiding the biopsy. However, due to high degree of radiation exposure its role is limited.
MRI is the useful modality for the early diagnosis of marrow changes in absence of identifiable lytic lesions on X-ray or CT scan. Nowadays it emerged as most sensitive modality for detection of focal or diffuse involvement in the spine as well as the extra-axial skeleton [3, 4]. Typical multiple myeloma lesions appear hypointense on T1W and hypertensive on T2W images. Post-contrast study shows homogeneous enhancement of the osseous lesions as well as extra-osseous soft tissue. However, sometimes lesions appear hypointense on T2W images depending upon the plasma cell percentage (between 10-50%) [5]. Major advantage for the MRI is no radiation exposure, so it can be used for the follow-up imaging.
On FDG-PET multiple myeloma shows high metabolic activity. It is an important tool for staging and prognosis of multiple myeloma due to its ability to pick up metabolic activity, extra-medullary disease and secondary lesions that are not attributable to multiple myeloma [6]
Take home message: In multiple lytic lesions in the axial and appendicular skeleton with involvement of the mandible, multiple myeloma should be first in the differential consideration.
Differential Diagnosis List
Final Diagnosis
Multiple myeloma
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
T1W axial

T1W post-contrast axial

T1W post-contrast coronal

CT guided tru-cut biopsy

T2W axial

T2W sagittal
T1W post-contrast coronal

FDG PET image

1. Imaging Findings
Based on the cranial MRI, chest CT, and PET-CT images provided by the patient, the following major imaging characteristics are observed:
- MRI (Cranial): In the skull base and petrous part of the temporal bone, there is evidence of localized bone destruction or occupying lesions. In certain areas, T1-weighted sequences show low signal intensity, while T2-weighted sequences exhibit isointense or slightly hyperintense signals, with uniform enhancement after contrast administration. Suspected soft tissue components in the skull base and parts of the cranium suggest possible osteolytic lesions with local extramedullary extension.
- CT (Chest): Varying degrees of reduced bone density and local osteolytic lesions are observed in the thoracic vertebrae and ribs. In some areas, lesions appear to breach the cortex externally. Although no evident fracture lines are visible on the CT images, there is a potential risk of fracture. A possible sternal puncture or biopsy trajectory is also indicated.
- PET-CT: Multiple skeletal hypermetabolic lesions are noted, especially affecting the spine, ribs, and skull in the axial skeleton, indicating highly metabolic osteolytic changes consistent with multifocal lesions.
Laboratory results show decreased hemoglobin (Hb) (9 g/dL) and significantly elevated serum calcium (15 mg/dL), which is considered severe hypercalcemia (generally >14 mg/dL is regarded as severe). Combined with clinical symptoms such as headache and diplopia, these findings suggest the possibility of a systemic disease involving the skull base and cranial nerves.
2. Potential Diagnoses
Based on the above imaging findings, along with the patient’s laboratory results and clinical symptoms, the following diagnoses or differentials are possible:
-
Multiple Myeloma
Rationale: Commonly seen in middle-aged and older patients, often presenting with anemia, hypercalcemia, osteolytic bone destruction, and bone pain. Serum protein electrophoresis may show elevated M protein. MRI can reveal bone marrow infiltration and local soft tissue masses. -
Metastatic Bone Tumor
Rationale: Osteolytic lesions can also occur in bony metastases from certain solid tumors (e.g., breast cancer, lung cancer). However, identification of a primary lesion, lack of specific M protein elevation, and consideration of clinical and immunological tests are necessary for comprehensive diagnosis. -
Lymphoma Bone Invasion
Rationale: Certain types of non-Hodgkin’s lymphoma may involve the bone. Imaging can sometimes display mixed osteolytic and sclerotic features. Pathological biopsy is required for differentiation.
3. Final Diagnosis
Taking into account the clinical presentation (anemia, headache, diplopia), laboratory findings (marked hypercalcemia, reduced hemoglobin), imaging characteristics (multifocal osteolytic bone destruction, evidence of bone marrow infiltration), as well as hints from electrophoresis and bone marrow aspiration results, the most likely diagnosis is:
Multiple Myeloma.
If there is still uncertainty or a need for special subtype clarification, further bone marrow biopsy and tests such as immunofixation electrophoresis and free light chain assays can be performed to confirm the diagnosis and assess staging.
4. Treatment Plan and Rehabilitation
(1) Treatment Plan
- Chemotherapy and Targeted Therapy: Combination regimens including alkylating agents, proteasome inhibitors, and immunomodulators can significantly improve disease progression.
- Supportive Care: This includes correction of hypercalcemia (intravenous fluids, bisphosphonates), symptomatic management of anemia, and infection prevention.
- Management of Bone-related Complications: For sites with evident structural damage and a high risk of pathological fractures, interventions such as vertebroplasty, surgical fixation, or radiotherapy may be considered to stabilize local lesions.
- Hematopoietic Stem Cell Transplantation: Autologous stem cell transplantation may be an option for eligible patients to improve outcomes.
(2) Rehabilitation and Exercise Prescription
- Rehabilitation Goals: Alleviate bone pain, enhance activities of daily living, prevent further fractures, and improve overall functional status.
- Exercise Prescription Principles (FITT-VP):
- Frequency: 3-5 times per week, adjusted according to the patient’s endurance and pain level.
- Intensity: Start with low intensity (e.g., slow walking, stretching), avoiding excessive weight-bearing or vigorous movements.
- Time: 15-30 minutes per session initially, gradually increasing to 30-45 minutes as tolerated.
- Type: Emphasize low-impact aerobic activities (such as walking or using a stationary bike), supplemented by low-intensity resistance training (using resistance bands or light dumbbells). High-load or spine-jarring activities should be avoided.
- Progression: Increase exercise duration and intensity slightly every 2-4 weeks, provided there is no cyanosis, severe dyspnea, or significant worsening of bone pain.
- Volume and Personalization: Begin with a smaller total exercise volume, then adjust individually as the patient recovers. Combine with nutritional support to prevent exacerbation of hypoproteinemia or anemia.
- Safety Precautions: Given the patient’s fragile bones, falls and high-impact exercises must be avoided. If severe pain, dizziness, or fatigue occurs, exercise should be stopped immediately, and medical consultation is advised.
Disclaimer
This report is a reference medical analysis based on the limited information provided and cannot replace a professional consultation or a physician’s opinion. Specific treatment and rehabilitation plans must be tailored to the patient’s actual clinical condition under the guidance of a qualified medical professional.
Human Doctor Final Diagnosis
Multiple myeloma