Role of ethambutol scintigraphy in uncertain cases of tuberculous osteomyelitis



Clinical History
A 24-year-old female patient was referred to our hospital with a right knee pain and movement difficulties after a fall one year before. The patient had no complaints of fever, dyspnea, or cough. In 2014 she was treated for lung tuberculosis, with a completed treatment during nine months.
Imaging Findings
The patient had plain radiography, knee-MR, bone and ethambutol scintigraphy. Radiograph of the right lower limb shows lytic lesions in the epi-metaphyseal of the proximal right tibia, with ill-defined margin, wide zone transition, and no periosteal reaction, which was suspected as a primary bone tumour.
Knee-MR showed multiple hypointense lesion in T1-WI, hyperintense in T2-WI at the lateral condyle of the right tibia and right femur, also the proximal right fibula. They showed diffuse enhancement after contrast injection with some areas showed peripheral enhancement, which showed an abscess formation.
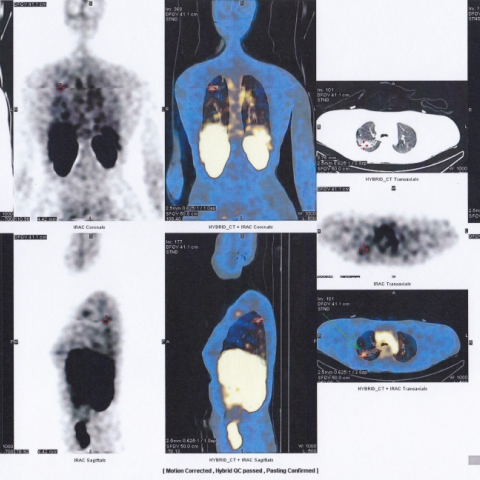
Bone scintigraphy using technetium-99m–labeled methylene diphosphonate (99m-Tc MDP) showed radioactivity uptake in the right tibia, which is not a likely site for bone metastases. Afterwards, they patient had ethambutol scintigraphy using 99m-Tc Ethambutol which showed radioactivities uptake in a B2 segment of the right lung and lateral condyle of the right tibia. This shows an active tuberculous process.
Discussion
Tuberculosis (TB) is still a global health problem despite the availability of various diagnostic modalities and effective antituberculous regiment [1, 2, 3, 5]. Therefore, a fast and accurate diagnosis becomes the key element in eliminating TB [5].
TB can involve pulmonary and extrapulmonary sites. Musculoskeletal system involvement shows only in 1-3% of cases, with extra-spinal manifestations being tuberculous arthritis, osteomyelitis and soft tissue TB. Femur, tibia and small bones of the hands and feet are the most likely sites for extra-spinal musculoskeletal TB and present usually as a solitary lesion [1, 3].
Bone involvement in TB usually results from hematogenous spread from a primary focus, usually the lung or the lymphatic system [2]. The mycobacterium would deposit in the metaphyses, and cause bone destruction, transphyseal spread and joint involvement [2, 3]. Early diagnosis and prompt treatment are critical to avoid bone destruction and joint deformity [3, 4]. However, clinical presentations and signs are often unspecific and insignificant, thus more difficult to diagnose. Therefore, radiologist must be aware of the possibility since further investigations can be based on radiographic findings [1, 3].
In plain films, tuberculous osteomyelitis shows osteolytic foci with ill-defined borders in the metaphyses, with or without a cortical breakthrough and various amounts of sclerosis [1, 3]. CT scan can show early bone destruction and sequestrum formation [3, 4]. However, MR imaging is the modality of choice since it demonstrates intraosseous and soft tissue involvement (abscess, fistula and sinus tracts) [4]. Marrow changes appear as hypointense on T1-WI and hyperintense on T2-WI, with homogenous or heterogenous enhancement after contrast injection [3, 4]. An interosseous abscess can show peripheral enhancements [6].
Radionuclide emission-based nuclear medicine, using antitubercular drug Ethambutol (EMB) labelled with 99m-Technetium, is a non-invasive, sensitive and specific method to detect and locate tubercular lesion at an early stage of the disease in any anatomical site. It shows a high labelling efficiency (>85%) with in-vitro and in-vivo stability and shows a consistent biodistribution and pharmacokinetic parameters with the original drug, which suggested that 99Tc-EMB was safe for diagnostic purposes [5].
In this case, MR imaging has shown osteomyelitis of the right proximal tibia and distal femur. The bone biopsy did not show any malignancy but spur formation and exostosis. Since it failed to conclude the diagnosis, the patient was referred to nuclear imaging. A positive ethambutol scintigraphy, combined with increased ESR and positive Mantoux test, confirmed a tuberculous osteomyelitis. The patient was treated once again with tuberculosis regiment. In uncertain cases, ethambutol scintigraphy can aid to diagnose tuberculosis.
Differential Diagnosis List
Final Diagnosis
Tuberculous Osteomyelitis
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Conventional X-ray


MRI of the Knee




MRI of the Knee




Ethambutol scintigraphy
Bone scan

Radiological Findings
Based on the provided X-ray and MRI images, there is evidence of bone destruction around the right knee joint (primarily involving the proximal tibia and distal femur). Irregular cortical changes are observed, with a blurred boundary and partial hyperplasia or spur formation. MRI shows abnormal bone marrow signals, presenting as low signal intensity on T1-weighted images and high signal intensity on T2-weighted images, with a certain range of soft tissue involvement. Abnormal signal shadows can also be seen near the articular surface, suggesting possible involvement of the joint and surrounding soft tissues. The overall radiological features are consistent with chronic osteomyelitis or tuberculosis infection leading to bone destruction.
Possible Diagnoses
- Osteoarticular Tuberculosis (Tuberculous Osteomyelitis/Arthritis): The patient has a history of pulmonary tuberculosis. MRI findings are in line with tuberculosis-related bone destruction and soft tissue involvement. Clinically, there is also an elevated ESR and a positive tuberculin skin test, supporting this diagnosis.
- Bacterial (Non-Mycobacterium Tuberculosis) Osteomyelitis: Chronic osteomyelitis can present with bone destruction and soft tissue changes on imaging. However, the patient lacks obvious acute purulent symptoms, and given her history of tuberculosis, this is less likely.
- Bone Tumor or Tumor-like Lesion: Osteosarcoma, chondrosarcoma, or other malignancies can sometimes manifest as lytic or mixed destructive lesions. However, pathological results show no malignant cells, and clinical and laboratory data suggest a higher likelihood of infection.
Final Diagnosis
Considering the patient is a young female with a history of pulmonary tuberculosis, long-standing clinical symptoms (right knee joint pain and restricted motion), laboratory tests (positive Mantoux test, elevated ESR), absence of malignant cells in bone biopsy, and positive radiotracer findings (e.g., radiolabeled ethambutol), the most likely diagnosis is Right Knee Tuberculous Osteomyelitis (Osteoarticular Tuberculosis).
Treatment Plan and Rehabilitation
- Anti-Tuberculosis Therapy: According to national and international guidelines for tuberculosis treatment, initiate a standard anti-tuberculosis regimen (which may include isoniazid, rifampin, pyrazinamide, and ethambutol). The duration is generally at least 6–9 months, and may be extended based on drug resistance patterns and the rate of lesion healing. Adherence to specialist instructions is essential.
- Surgical Intervention: If there is significant bone destruction or joint deformity, an evaluation should be made regarding debridement, drainage, or bone graft repair. Specific indications will be determined by orthopedic or joint specialists.
- Rehabilitation and Exercise Prescription:
- During the acute inflammatory phase or when pain is significant, limit weight-bearing appropriately and maintain immobilization or partial weight-bearing of the affected limb. Use assistive devices to reduce joint pressure.
- Once symptoms improve, gradually start range-of-motion exercises, progressing from passive to active movements to prevent joint stiffness and muscle atrophy.
- In the stable phase, add muscle-strengthening exercises—such as isometric or low-resistance workouts for the quadriceps and other surrounding muscles—3–4 times per week. Gradually increase resistance and training duration (e.g., start with 10 minutes each session, increase by 2 minutes weekly).
- During the later stages of rehabilitation, moderate-intensity aerobic exercises (e.g., cycling, swimming) can be performed 3–5 times per week, 20–30 minutes each session, aiming for a subjective feeling of slightly strenuous effort. Adjust frequency and duration progressively (following the FITT-VP principle: Frequency, Intensity, Time, Type, Progression, and Individualization) to balance cardiovascular health and joint protection.
- Avoid excessive load-bearing and high-impact exercises throughout the process. Only consider increasing activity type and intensity once bone and joint function have adequately recovered.
Disclaimer
The above report is for reference only and cannot replace an in-person consultation or professional medical opinion. Patients should consult a qualified specialist for specific diagnosis and treatment, and should conduct rehabilitation training under professional guidance.
Human Doctor Final Diagnosis
Tuberculous Osteomyelitis