Rare case of primary synovial chondromatosis of the shoulder joint with suspected traumatic aetiology



Clinical History
A 40-year-old male patient presented to the GP in March 2008 with a history of recurrent left shoulder dislocations over the past four years.
Physical examination was unremarkable. Outpatient plain radiograph and an MRI was performed, but the patient did not attend follow-up appointments.
Imaging Findings
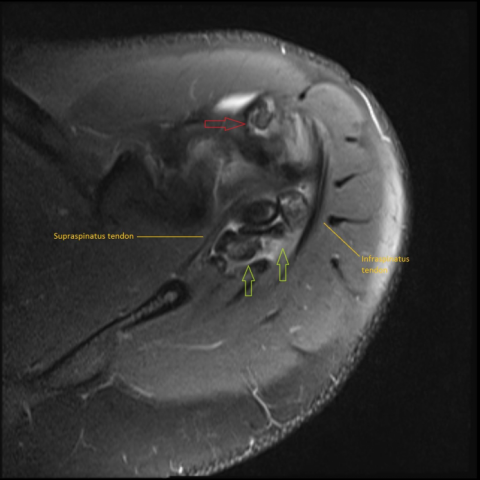
Initial plain radiography (Fig. 1) showed calcification in the region of the supraspinatus and a slightly loose body inferior to the glenoid but no fracture or osteoarthritis. During the follow-up appointment in August 2008, MRI was performed and showed subcortical cystic degeneration in the humeral head and features of synovial chondromatosis (Figs. 2, 3) and small loose bodies along the biceps tendon and supraspinatus tendon.
The patient did not attend the follow-up appointments and returned eight years later when a repeated plain radiography (Fig. 4) showed multiple intra-articular loose bodies around the humeral head. A subsequent MRI in June 2016 demonstrated progression, with multiple large loose bodies, supraspinatus tear and partial thickness infraspinatus tear (Fig. 5) that were visible along with multiple loose bodies within the suprapinatus tendon and the biceps tendon sheath (Figs. 6a, 6b, 7a, 7b).
Discussion
Primary synovial chondromatosis (PSC) is an uncommon condition characterised by metaplasia of the chondroid along with multinodular proliferation of the synovial lining which can be of a diarthrodial joint, tendon sheath or bursa. The definite aetiology is unknown, although it was proposed that it is due to the reactivation of residual embryonal cells [3] present in the related area and, in some literature, trauma has been reported as the cause [2].
It is generally believed that PSC is not a neoplastic process, but a metaplastic process initiated by trauma or chronic irritation [6, 7, 8]. An animal study showed that synovial chondromatosis has a relationship with osteoarthritis secondary to trauma [8]. It has a male predominance with an incidence of 1:100000 and it mostly occurs afresh in a healthy joint [4]. The most common joint involved is the knee joint, followed by the hip joint. Involvement of the shoulder joint is uncommon and extra articular involvement is rare [5]. Generally, these patients have chronic pain and stiffness in the affected joint [1].
Diagnosis is usually straightforward with plain radiographs which show osteochondral loose bodies distributed within the joint capsule, but which rarely involve the bursae or tendon sheath [9]. Additional imaging aids the diagnosis in atypical cases and also identifies any associated abnormalities.
In this case, MRI was crucial in demonstrating the location of the loose bodies within the supraspinatus tendon which could have been mistaken for calcific tendinitis.
This was an unusual case of PSC effecting the shoulder joint along with tendon involvement and a causal relationship due to trauma and repeated irritation was hypothesised. Treatment is mainly aimed at symptomatic relief and, in complicated cases, surgical intervention may be necessary.
A combination of imaging techniques is required to reach the diagnosis and this particular case also highlights the importance of plain radiographs, particularly in musculoskeletal pathology. In this case, the diagnosis was made based on the radiological findings and the clinical history. The patient refused any surgical intervention and histological confirmation was not possible.
Differential Diagnosis List
Final Diagnosis
Primary synovial chondromatosis
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
X-Ray of the left shoulder AP view

MRI of the left shoulder (Sagittal view PDFS)

MRI of the left shoulder (coronal view PDFS)

X- ray left shoulder AP view

MRI left shoulder (coronal view PDFS)


MRI left shoulder ( Axial view, PDFS)
MRI left shoulder (Sagittal view, PD weighted)


Medical Imaging Analysis Report
I. Imaging Findings
The patient is a 40-year-old male with a history of recurrent left shoulder dislocations. Based on the provided shoulder X-ray and MRI images, the following features are noted:
- Shoulder X-ray plain film: Multiple high-density shadows around the shoulder joint presenting as small nodular or round-like shapes. Some are located beneath the acromion or near the humeral greater tuberosity, possibly indicating intra-articular or peri-tendinous loose bodies.
- MRI sequences (T1, T2-weighted images, and others) show multiple cartilage-like nodules around the shoulder joint cavity and in the rotator cuff tendons (particularly evident in the supraspinatus tendon region). Some exhibit slightly elevated or isointense signals, with mild synovial thickening around them and adjacency to synovium or tendon tissue, potentially accompanied by tenosynovial/synovial hyperplasia.
- No significant widespread bony destruction is observed. The local rotator cuff tendons remain structurally intact overall, but display certain tendon pathology signals (e.g., high signal areas in the supraspinatus tendon), suggesting repeated irritation or chronic injury.
II. Potential Diagnoses
Based on the clinical history (recurrent dislocation, chronic shoulder pain/discomfort) and imaging findings (multiple loose bodies or cartilaginous nodules), the following diagnoses are primarily considered:
- Primary Synovial Chondromatosis (PSC)
- Characteristics: Formation of cartilage-like nodules on the synovial surface, most commonly seen in large joints such as the knee or hip; less commonly in the shoulder. On imaging, multiple cartilaginous bodies may be identified, sometimes showing calcification or ossification. The etiology may be related to chronic irritation or trauma.
- Enchondroma/Cartilaginous lesions leading to shoulder joint loose bodies
- Characteristics: Usually a benign bony or cartilaginous lesion that may detach or induce changes in adjacent tissues due to joint activity. However, multiple lesions involving and thickening the synovium are less common than in PSC.
- Calcific Tendinitis (Calcium Deposits in Tendon)
- Characteristics: Commonly involves the rotator cuff tendons (especially the supraspinatus tendon), presenting as calcific foci and causing shoulder pain. Typically, high signal or high-density areas are seen within the tendon or adjacent soft tissues, but the presentation of multiple discrete bodies involving the synovium is atypical.
III. Final Diagnosis
Based on the patient’s age, history of recurrent shoulder dislocations, and imaging findings showing multiple cartilaginous bodies and synovial/tenosynovial changes, the most likely diagnosis is:
Primary Synovial Chondromatosis (PSC)
This diagnosis aligns with the patient’s long-standing shoulder instability, history of repeated trauma/irritation, and MRI findings of multiple cartilaginous nodules within the synovium. Owing to the patient’s refusal of surgical intervention, pathological confirmation could not be obtained; nonetheless, considering the overall imaging appearances and clinical features, PSC remains the most likely diagnosis.
IV. Treatment Plan and Rehabilitation
General Treatment Strategies:
- Conservative Treatment: For patients with mild symptoms or limited lesion size, anti-inflammatory and analgesic medications (e.g., NSAIDs) can be used to control pain, combined with physical therapy (e.g., heat therapy, ultrasound therapy) to relieve discomfort.
- Surgical Treatment: Indicated for patients with severe symptoms, significantly reduced joint range of motion, or large loose bodies when conservative treatment is ineffective. Arthroscopic surgery may be considered to remove loose bodies and partially resect the synovium.
Rehabilitation/Exercise Prescription Recommendations (FITT-VP principle):
- Frequency: 3-5 rehabilitation sessions per week, gradually increasing to once daily or every other day based on symptom relief.
- Intensity: Start with low-intensity active/passive joint movements (e.g., small-range abduction, adduction, flexion) and avoid large rotational or weight-bearing movements. Gradually progress to moderate-intensity shoulder strengthening as tolerated, considering pain levels and joint stability.
- Time: Each session should last about 20-30 minutes, divided into segments to avoid continuous prolonged training.
- Type: Early-stage exercises may include gentle range-of-motion activities (e.g., wand exercises, towel-assisted extension, pendulum exercises). Later, as pain decreases and function improves, resistance band or light dumbbell exercises can be introduced to strengthen the rotator cuff.
- Progression: Increase range of motion and resistance gradually as symptoms permit. If tolerated, more advanced functional moves (e.g., wall push-ups, bent-over rows, external rotation exercises with resistance) can be attempted.
- Volume: When maintaining low to moderate intensity, perform 10-15 repetitions per movement for 2-3 sets, with 30-60 seconds of rest between sets. Adjust according to clinical status and endurance.
Precautions: If significant pain exacerbation, joint instability, or recurrent dislocation occurs, suspend training and seek reevaluation. In patients with osteoporosis or compromised cardiopulmonary function, pay special attention to exercise intensity and posture to prevent falls or excessive cardiovascular stress.
Disclaimer: This report is for reference information only and cannot substitute for an in-person medical consultation or professional physician advice. Specific diagnoses and treatment plans must be determined by professional physicians based on the patient’s detailed medical history, physical examination, and other relevant tests.
Human Doctor Final Diagnosis
Primary synovial chondromatosis