


A 15-year-old boy without medical history presented to the emergency department with back pain, difficulty to walk, and urinary malfunction. The neurological examination showed paraparesis and myoclonus of the left lower limb as well as hypoesthesia up to T10.
A contrast-enhanced MRI and CT of the dorsal spine were performed.
MRI showed a heterogeneous multi-loculated cystic lesion located in the posterior arch of T5, T6, with extension in the T5 vertebral body and mass effect on the adjacent spinal cord. This lesion had multiple cavities with fluid-fluid levels, appeared in low signal intensity on T1-weighted images (Fig. 3) and in mixed low and high intensity on T2 FAT SAT-weighted images (Fig. 1 and 2). The enhanced series of this study (T1 FAT SAT GD, Fig. 4) demonstrated rim enhancement of the fluid-fluid levels cavities.
CT showed an expansive multi-loculated lytic lesion of the posterior arch of T5 and T6, with peripheral calcifications (Fig. 5) and rim enhancement of the cavities after contrast injection (Fig. 6). It also revealed the subperiosteal origin of the lesion with secondary involvement of the cortical bone.
Aneurysmal bone cyst (ABC) is a benign bone lesion of unknown origin, first described in 1942 by Jaffe and Lichtenstein. It is a relatively rare lesion that represents 1.4%–2.3% of primary bone tumours [1]. The spine is involved in 3%–20% of cases [1].
Although benign, an ABC has the potential to grow acutely, and can cause a lot
of swelling and pain while disrupting the growth plates, pathological fractures, and neurological manifestations.
ABC primarily occurs in the first two decades of life, but can occur at any age, with slight women predominance [2].
In 29%–35% of cases, a pre-existing lesion can be identified. The most common of these is giant cell tumour, osteoblastoma, angioma, and chondroblastoma.
The cervical spine is affected in 22% of cases, the thoracic spine in 34%, the lumbar spine in 31%, and the sacrum in 13% [3]. Spinal involvement is typically in the posterior elements, although extension into the vertebral body is also common [3].
Histologically, ABC is typically characterised by blood-filled cystic spaces separated by a spindle cell stroma with osteoclast-like giant cells and osteoid or bone production. The lack of anaplasia in all the tissue components strongly argues against a malignant tumour [1].
CT and MR imaging typically show a well-defined lesion with internal septation and enhancement after injection. Hudson et al. [4] show that in 35% of ABCs have fluid-fluid levels at CT. Fluid-fluid levels are indicative of haemorrhage with sedimentation, better demonstrated on MRI. They may have increased signal intensity due to methaemoglobin on T1.
Different treatments have been proposed in the literature such as pre-operative selective arterial embolisation, intralesional excision curettage, bone grafting, intralesional drug injections (steroid and calcitonin), and radiation [1, 2].
In our case, the aneurysmal bone cyst was first treated by arterial embolisation followed by sclerotherapy. Treatment was completed two months later by total surgical resection along with dorsal spondylodesis T3-T8. No residual lesion was found on the MRI performed 12 months after surgery.
Although ABC is a benign lesion, one should bear in mind it can be locally aggressive (e.g., responsible for spine compression) and that recurrence rates up to 50 % after resection have been reported [2].
Aneurysmal bone cyst.
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.



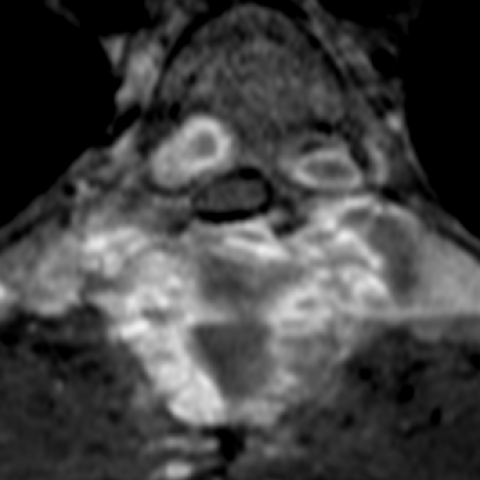
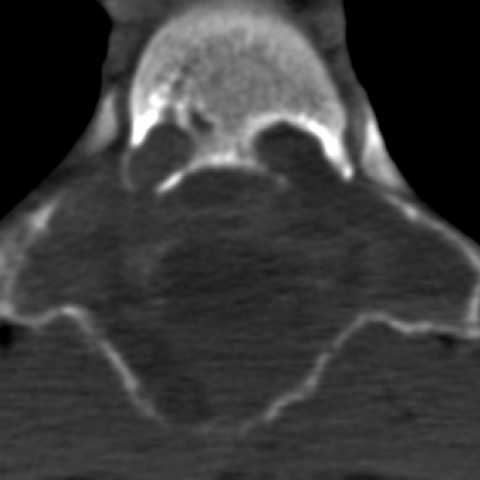

From the provided MRI and CT images, an obvious expansile bony lesion is visible in the posterior aspect of the vertebral body and pedicle region, showing a cystic appearance with internal septations and a multi-chamber characteristic. In some MRI sequences, fluid-fluid levels of different signals are observed, indicating intralesional hemorrhage and possible stratification. The lesion has relatively clear margins, with a degree of bony expansion and mild erosion of the surrounding cortical bone, protruding slightly into the spinal canal and causing spinal cord compression. The surrounding soft tissue shows varying degrees of swelling, but no obvious solid mass signal is detected.
The lesion is located in the posterior structures and part of the thoracic vertebrae (T3–T8). Local narrowing of the adjacent spinal canal is noted, correlating with clinically observed signs of spinal cord compression, including weakness in both lower limbs, difficulty walking, and possible bladder dysfunction.
Based on the patient’s adolescent onset, the expansile lytic lesion with fluid-fluid levels observed on MRI and CT, and the surgical/pathological findings of a hemorrhagic cavity, pathological bone tissue, and multinucleated giant cells, a clear diagnosis of an Aneurysmal Bone Cyst (ABC) is established.
During the postoperative period or after treatment stabilization, rehabilitation should focus on enhancing spinal stability, improving lower limb strength, and restoring normal gait. A gradual and individualized approach is essential, following the FITT-VP principles (Frequency, Intensity, Time, Type, Progression, Individualization). The recommended plan is as follows:
During rehabilitation, closely monitor pain, numbness, or any decline in muscle strength. If significant discomfort or worsening neurological symptoms occur, revisit the physician promptly to adjust the plan.
Disclaimer: This report is based on the provided information for reference purposes and does not replace an in-person consultation or professional medical advice. A specific diagnosis and treatment plan should be made according to the actual situation and under the guidance of a qualified physician.
Aneurysmal bone cyst.