


A 23-year-old male patient presented with abdominal pain, nausea, vomiting, rectal bleeding and weight loss. A series of investigations were undertaken including sigmoidoscopy with biopsy, CT & MRI of the small bowel which all showed active colitis. Multifocal lytic lesions in ilium bilaterally were picked up on CT incidentally.
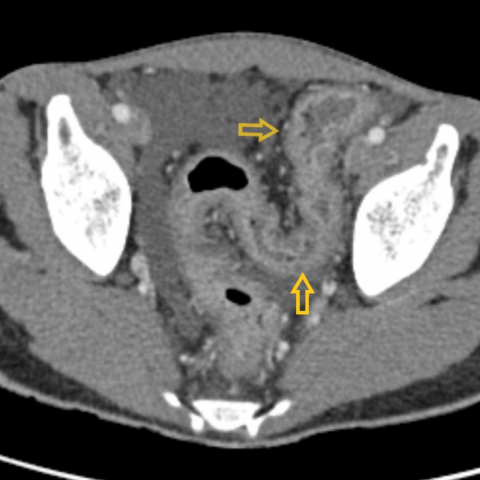
CT examination showed active inflammation in sigmoid and descending colon in the form of wall thickening, an imaging hallmark of ulcerative colitis (UC) [5]. Bilateral sacroiliitis was noted along with an unexpected finding of discrete lytic lesions with a fluid density in both iliac bones.
MRI study of the bowel revealed similar findings and confirmed the cystic nature of the osseous lytic lesions.
Radiographically brown tumours are discrete low attenuating cystic lesions [5] with irregular outline on CT & fluid signal on MRI [1]. These can occur frequently in the pelvis, ribs, and clavicles [1].
Brown tumours may simulate giant cell tumour (GCT), giant cell granuloma (GCG) and metastatic carcinoma [1], knowledge of certain key imaging features can however aid in differentiation. On imaging, GCT lesions are usually epiphyseal & eccentric with pseudotrabeculations, GCG lesions are trabecular with sharp margins and metastatic lesions exhibit surrounding invasion [1].
Brown tumours are non-neoplastic lesions, seen as a musculoskeletal manifestation of hyperparathyroidism. They occur more commonly in primary hyperparathyroidism than in secondary hyperparathyroidism [4]. Primary hyperparathyroidism is characterised by a spontaneous abnormal secretion of parathyroid hormone (PTH) and is diagnosed clinically by the presence of hypercalcaemia with increased PTH levels [2]. Gastrointestinal manifestations mostly include vague abdominal complaints and disorders of the stomach and pancreas [3], and do not include involvement of the bowel.
This case had clinical symptoms suggestive of ulcerative colitis (UC), which was confirmed on sigmoidoscopy. However, the clinical diagnosis of primary hyperparathyroidism was not present at the time of radiological imaging. Patient was advised to undergo CT abdomen to delineate the complete extent of large bowel involvement.
The presented case is one of its kind, because in this case brown tumours were seen in a patient diagnosed with UC initially and hyperparathyroidism was subsequently confirmed.
To investigate further, patient’s serum calcium and PTH levels were checked. Results showed hypercalcaemia and increased levels of PTH, consistent with primary hyperparathyroidism in the background of UC. Patient did not have any bone complaints. The hypercalcaemia is asymptomatic in more than 90% of patients with primary hyperparathyroidism [3].
On our literature search, we found no article describing an observation of brown tumours co-existing with UC. Although there are reports of co-existing hyperparathyroidism and ulcerative colitis, most had parathyroid adenoma [6-9] and none had brown tumours.
The initial report of hyperparathyroidism in a patient of ulcerative colitis was documented by Grek & Senior in 1961 [8]. It is postulated that as the calcium levels are reduced in longstanding UC, possibly long term steroid usage can cause an increase in quantities of PTH, which can result in either hypoparathyroidism or hyperparathyroidism (adenoma formation). However, definite pathophysiology still remains unclear.
UC and hyperparathyroidism can co-exist in a same individual and this is being increasingly reported [6-9]. Hence, a clear look out for any additional findings on imaging should be attempted. This case showed lytic lesions in iliac bones in addition to UC findings, & prior knowledge of the coexistence of UC & primary hyperparathyroidism instigated us to investigate further. Early detection & treatment can prevent a cascade of parathyroid crisis.
Brown tumours secondary to primary hyperparathyroidism on a background of ulcerative colitis
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.








The patient is a 23-year-old male with a history of abdominal pain, nausea, vomiting, bloody stools, and weight loss. He was confirmed by colonoscopy and biopsy to have ulcerative colitis (UC). During CT and MRI examinations, incidental multifocal lytic lesions were found in both iliac bones.
Based on the patient’s clinical history (ulcerative colitis) and laboratory results (hypercalcemia, elevated parathyroid hormone), the following differential diagnoses should be considered:
Considering the patient’s confirmed ulcerative colitis, multifocal lytic lesions on imaging, along with laboratory findings of hypercalcemia and significantly elevated PTH levels, and subsequent further testing, the most likely diagnosis is:
“Brown tumor caused by primary hyperparathyroidism in a patient with ulcerative colitis.”
If necessary, parathyroid ultrasound, nuclear imaging, or surgical exploration may be conducted to identify parathyroid adenoma. The bone lesions can be monitored or biopsied to rule out other pathologies.
Treatment Strategy:
1. Ulcerative Colitis Management: Focus on anti-inflammatory and immunomodulatory therapies, such as 5-aminosalicylic acid preparations, corticosteroids, immunosuppressants, and biologics. Specific medication regimens should be based on disease activity, previous treatment response, and patient tolerance.
2. Management of Primary Hyperparathyroidism: If a parathyroid adenoma is confirmed, surgical resection may be considered. If the patient is not a surgical candidate, management of calcium-phosphorus metabolism is required to reduce further bone destruction. Bisphosphonates and adequate vitamin D supplementation may be used for symptomatic relief.
3. Bone Lesions (Brown Tumors): Brown tumors often improve or stop progressing once parathyroid function is normalized. Surgical intervention may be considered if there is significant bone destruction or a high risk of pathological fracture.
Rehabilitation and Exercise Prescription (FITT-VP Principle):
Given that the patient has ulcerative colitis (which may flare up) and low bone mass or a risk of bone fragility, the exercise program should be mindful of both gut conditions and skeletal safety, adhering to a gradual and individualized approach.
Throughout the rehabilitation process, the patient should work closely with physicians and rehabilitation specialists, regularly monitoring serum calcium, PTH, bone density, and colonic status to make timely adjustments to both medical and exercise therapies.
Disclaimer: This report is a reference analysis based on the available information and should not be taken as the sole basis for diagnosis or treatment. It does not replace an in-person consultation or the opinion of a qualified medical professional. If you have any questions, please consult a specialist for further evaluation and treatment.
Brown tumours secondary to primary hyperparathyroidism on a background of ulcerative colitis