Calcific tendinopathy of the pectoralis major mimicking bony metastasis



Clinical History
A 77-year-old male patient with newly diagnosed prostate cancer attends for a Tc-99m bone scan, which lead to the suspicion of humeral metastasis. The patient was asymptomatic, with a mildly raised PSA and had a normal bone profile.
Imaging Findings
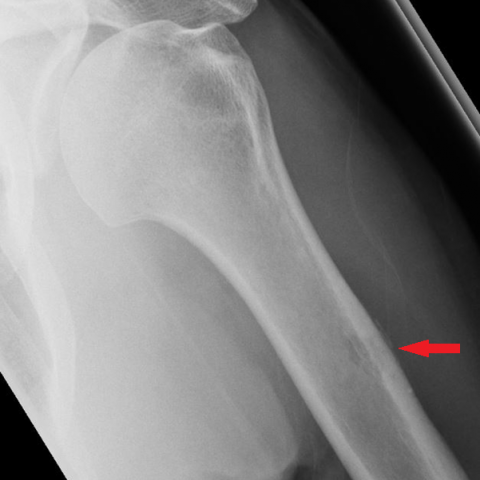
Bone scan revealed faint focal uptake in the left proximal humerus (Fig. 1). Initial radiograph showed a 'sclerotic lesion' at the area of bone scan uptake (Fig. 2). Subsequent radiographs demonstrated gradual resolution of the sclerotic focus, with new focal lysis and mineralisation away from bone which was initially interpreted as periosteal reaction (Fig. 3, 4). The rapid radiographic evolution raised suspicions of humeral metastasis. Shoulder MRI showed a small ovoid area of altered signal in the anterior humeral cortex corresponding to the abnormality seen previously, but no marrow oedema or soft tissue mass (Fig. 5, 6). Subsequent CT of the humerus showed a corresponding well-defined concave cortical remodelling but nil else (Fig. 7). No metastases were seen on CT chest/abdomen/pelvis. All imaging was subsequently reviewed by regional MSK/sarcoma radiologists and the diagnosis of calcific tendinopathy of the pectoralis major was made, and not bony metastasis. Biopsy was deemed unnecessary.
Discussion
Bony involvement is an uncommon, but well recognised, feature of calcific tendinopathy that may be confused with other pathologies, including malignancy [1-4]. The underlying pathophysiology is thought to be related to hypervascular inflammatory changes, with contributing effects of muscular traction, which induce focal resorption of the adjacent bone [3].
The tendinous insertion of the pectoralis major at the proximal humeral diaphysis is one of the commonest locations of calcific tendinopathy associated with osseous involvement [1]. To the best of our knowledge, this is the first report of pectoralis major calcific tendinopathy mimicking prostate cancer metastasis. The calcific deposit overlying the proximal humerus on the initial radiograph was misinterpreted initially as a sclerotic bony lesion. The rapid resolution of this, however, is unusual for a metastasis, but is often seen in the natural history of calcific tendinopathy. The remaining features of cortical erosion at the site of the pectoralis tendon insertion, mild uptake on scintigraphy and absence of a soft tissue mass are also recognised features of osseous involvement in calcific tendinopathy [1-4]. Although periosteal reactions have been reported in calcific tendinopathy [1], it was felt that the mineralisation away from bone seen in our case (Fig. 4) was perhaps more in keeping with calcific deposit within the pectoralis major tendon. More aggressive features that may be seen (not present in our case) include marrow oedema [1, 4] and enhancement of the surrounding tissues [4].
An important learning point from this case was the need to always obtain a second projection. Should a true lateral projection have been performed at the time of the initial radiograph, the reporting radiologist would have realised that the sclerotic lesion was not in fact intraosseous, but in the adjacent soft tissues, and thus would have avoided the need for subsequent MRI/CT to further investigate this.
Radiologists should be aware of the unusual appearances and sites of calcific tendinopathy, which in itself is a very common pathology. Biopsy was fortunately avoided in this patient, but if performed, chondroid metaplasia may be seen and the misdiagnosis of chondrosarcoma may be possible [4]. Recognition of this benign entity is therefore of utmost importance to avoid unnecessary biopsy with its inherent risks and patient distress.
Differential Diagnosis List
Final Diagnosis
Calcific tendinopathy of the pectoralis major tendon
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Technetium-99m bone scan

Initial plain radiograph of left shoulder

Plain radiograph obtained 2 weeks later

Plain radiograph obtained 5 weeks later
Axial T1-weighted MRI image

Coronal STIR MRI image

Axial CT image

Imaging Findings
This patient is a 77-year-old male with a recently diagnosed prostate cancer. A Tc-99m bone scan indicated increased radiotracer uptake in the proximal right humerus, commonly suggestive of a metastatic lesion.
However, subsequent X-ray, MRI, and CT imaging revealed:
• On the anteroposterior (AP) X-ray, a possible sclerotic change was seen near the metaphyseal region of the proximal humerus. Initially, it was misinterpreted as a sclerotic bony lesion. However, from other imaging angles, the calcification was found on the lateral cortex of the humerus, with a clear boundary from the surrounding soft tissue.
• MRI showed a ring-shaped or “circular” high-signal rim at the pectoralis major tendon insertion, with partial compression or mild erosion of the underlying cortex, but no obvious soft tissue mass and only minimal surrounding inflammatory changes.
• CT further confirmed a ring-shaped high-density calcification at the insertion of the pectoralis major tendon, along with cortical thinning or groove-like changes, lacking the typical invasive features of a malignant tumor.
• Although the patient’s serum prostate-specific antigen (PSA) was mildly elevated, bone-related biochemical indicators were normal. Clinically, there were no symptoms such as right shoulder pain.
Based on these imaging features and clinical information, the calcification appears more consistent with a benign soft tissue calcification accompanied by local bone changes.
Potential Diagnoses
- Metastatic Bone Lesion: Given the patient’s history of prostate cancer and the initial bone scan showing increased uptake in the humerus, a metastatic lesion—especially a sclerotic metastasis—must be considered. However, true metastatic lesions typically present with more apparent cortical destruction, and the central calcification does not usually form a distinct ring.
- Calcific Tendinitis (Pectoralis Major Tendon Insertion): The insertion of the pectoralis major tendon is a common site for calcium deposits, which can lead to mild cortical changes (erosion or destruction). These calcific deposits may undergo rapid partial or complete resorption, and on imaging, they can be mistaken for malignant lesions.
- Chondrosarcoma or Other Cartilaginous Tumors: If a biopsy reveals cartilaginous components, it could be misdiagnosed as a cartilaginous tumor. However, such tumors typically exhibit more significant bone destruction, expansive growth, and more pronounced clinical pain.
Final Diagnosis
Considering the patient’s age, background of prostate cancer, stable serum indicators, and imaging characteristics (ring-shaped calcification located in soft tissue, rapid changes, and no obvious intramedullary invasion), the most likely diagnosis is: Calcific tendinitis at the pectoralis major tendon insertion (with local bone changes), rather than metastatic bone disease.
Treatment and Rehabilitation Plan
1. Therapeutic Strategy:
• Conservative Treatment: In cases with minimal or no symptoms, observation along with nonsteroidal anti-inflammatory drugs (NSAIDs) for symptomatic relief is advised. Physical therapies (e.g., ultrasound therapy, warm compresses) may help accelerate resorption of the calcified deposit.
• Injection Therapy: If pain is significant, consider local injection of corticosteroids or ultrasound-guided aspiration and lavage of the calcific deposit.
• Surgical Indications: Surgery to remove the calcification is considered only when conservative measures fail or if quality of life is significantly impaired by symptoms. Since this patient is asymptomatic, surgical intervention is not currently indicated.
2. Rehabilitation and Exercise Prescription (Following the FITT-VP Principle):
• Frequency: 3-4 sessions per week focusing on aerobic exercise and shoulder functional training.
• Intensity: Start with low-intensity activities (e.g., gentle shoulder exercises, active or assisted movements). Gradually increase resistance or strength training as tolerance improves.
• Time: About 20-30 minutes per session, possibly broken into intervals. Each set of stretching or strength exercises lasts roughly 10-15 seconds.
• Type: Emphasize shoulder joint mobility, light resistance, and stretching exercises. Avoid vigorous throwing or high-impact abduction movements.
• Volume: Gradually increase exercise volume. For instance, begin with simple arm swings or pendulum movements of the affected shoulder, then incorporate resistance bands or light dumbbells as tolerated. Adjust according to pain or fatigue levels.
• Progression: Expand the range of motion and introduce heavier loads as symptoms are controlled and strength returns. If pain worsens or discomfort appears, reduce intensity or pause and seek medical advice.
• For older adults, pay attention to baseline cardiopulmonary and bone health, proceed gradually, and ensure safety.
Disclaimer:
This report is based on the patient’s current medical history and imaging findings and is provided for medical reference only. It is not a substitute for an in-person medical consultation or professional opinion. If any questions arise or symptoms worsen, please seek appropriate medical evaluation and any necessary follow-up examinations or treatments.
Human Doctor Final Diagnosis
Calcific tendinopathy of the pectoralis major tendon