


69-year-old male patient with history of diffuse large B cell lymphoma (treated 2006/2014). Prior history of diabetes mellitus, degenerative spinal disease and neuropathy (dysphagia and mononeuritis multiplex) post chemotherapy treated with intravenous immunoglobulin. Presents with new onset back and right hip pain investigated with [18F]-Fluorodeoxyglucose–Positron-Emission Tomography/CT (FDG PET/CT) scan.
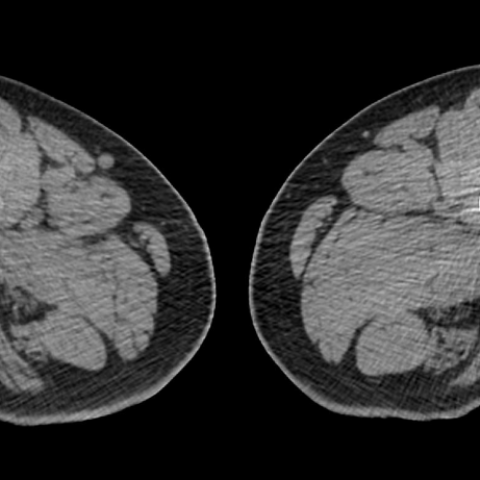
Maximum intensity projection image from FDG PET/CT showed linear intense tracer uptake within pelvis on right side and also demonstrated a lack of abnormal activity elsewhere in the body including absence of FDG-avid lymphadenopathy (Fig. 1). Axial CT image demonstrated fusiform thickening along right lateral pelvic side wall suggesting diffuse enlargement of the obturator nerve (Fig. 2). Reformatted PET/CT image demonstrated intense linear FDG uptake along the enlarged right obturator nerve as well as in its L4 nerve root (Fig. 3). Axial CT image at the level of proximal thigh shows denervation atrophy of adductor and gracilis muscle (Fig. 4). Follow up CT scan performed after targeted radiotherapy revealed interval reduction in size of thickened obturator nerve (Fig 5).
Background:
Neurolymphoma is a rare extranodal manifestation of lymphoma reflecting intraneural infiltration of malignant lymphocytes. Neurolymphoma likely represents an isolated focus of disease limited to the peripheral nervous system, either as the primary manifestation or as the sole site of recurrence. [1]
Clinical Perspective:
The clinical features of neurolymphoma are nonspecific, but patients often present with pain and sensory motor involvement. Motor weakness is usually a late feature [1]. A high index of suspicion is required as the presenting symptoms of this condition are varied (including plexopathy, mononeuritis multiplex, foot drop, radiculopathy, and cranial nerve palsies) and a number of differential diagnoses need to be considered (e.g. leptomeningeal lymphomatosis, nerve damage from herpes zoster, chemotherapy, nerve root compression, radiotherapy, lymphoma-associated vasculitis, and paraneoplastic syndromes). Imaging can help to differentiate it from other non-tumour conditions associated with lymphoma that also affect the peripheral nervous system. [2]
Imaging Perspective:
The MR imaging features of peripheral nerve lymphoma are nonspecific and may demonstrate a nodular or fusiform enlargement and T2 hyperintensity. The nerves typically demonstrate mild to moderate enhancement after the administration of gadolinium-based contrast agent, more than is typically seen with a nonspecific infectious or inflammatory cause; however, this can vary. MR imaging may fail to clearly demonstrate the length of nerve involved with lymphoma. [1]
FDG PET/CT is a promising imaging modality for the evaluation of neurolymphomatosis. It enables assessment of disease extent with a single whole-body examination because lymphoma typically demonstrates marked FDG uptake which is seen as intense linear uptake along the involved nerves. In addition, FDG PET/CT is particularly useful in depicting sites with the highest metabolic activity as a means of guiding biopsy when pathologic diagnosis is warranted, thereby reducing the rate of false-negative findings. Furthermore FDG PET/CT is ideally suited for the evaluation of response to therapy and to restage lymphoma. [1] In our case the diagnosis was made on the basis of clinical and radiological features as it was not possible to safely perform the biopsy. The patient was treated with radiotherapy with follow up CT scan showing a reduction in size of the thickened obturator nerve.
Teaching Points:
Peripheral neuropathies in patients with a known malignancy can represent a diagnostic dilemma. FDG PET/CT is a useful adjunct imaging because it facilitates the differentiation of malignant from benign disease. [1]
FDG PET/CT is useful in establishing the diagnosis as well as to guide biopsy and for assessment of response to therapy. [3]
Neurolymphomatosis of the right obturator nerve diagnosed on [18F]-Fluorodeoxyglucose–Positron-Emission Tomography/CT.
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.







Based on the patient's current FDG PET/CT images, the following observations can be made:
Considering the patient's medical history (previous diffuse large B-cell lymphoma, multiple neuropathies, chemotherapy-related neural complications) and the imaging findings, the following differential diagnoses are primarily considered:
Based on the patient’s history of diffuse large B-cell lymphoma, the significant FDG uptake in the local nerve bundle, and newly developed neuralgia or motor/sensory symptoms, the most likely diagnosis is:
Neurolymphomatosis.
If further confirmation is required, a biopsy or additional nerve conduction studies may be considered if feasible and safe. However, due to potential risks in certain areas (e.g., around the obturator nerve), clinical and imaging findings often guide the decision to initiate therapy and observe treatment response.
In view of the patient’s nerve damage and previous spinal degenerative changes, a rehabilitation program emphasizing “gradual progression, individualization, and safety” is recommended:
If the patient experiences severe pain, progressive numbness, or any worsening discomfort during training, medical evaluation should be sought promptly, and the plan should be revised accordingly.
This report is a reference analysis based on current medical data and imaging findings and cannot replace an in-person consultation or the individualized judgment of a professional physician. Any diagnosis or treatment decision must be made after considering the patient’s specific clinical situation, laboratory results, and specialist evaluations.
Neurolymphomatosis of the right obturator nerve diagnosed on [18F]-Fluorodeoxyglucose–Positron-Emission Tomography/CT.