An uncommon cause of an uncommonly diagnosed shoulder pain



Clinical History
A 31-year-old patient came with complaints of weakness of left upper limb for one month, with difficulty in lifting heavy objects. No history of numbness/tingling sensation. On clinical examination, power was 3/5 with sluggish triceps reflex. The sensory system was intact.
Imaging Findings
Prior to imaging, the patient underwent a nerve conduction study which was normal. Radiography of the left shoulder was unremarkable. Due to the persistence of complaints the patient underwent an MRI scan.
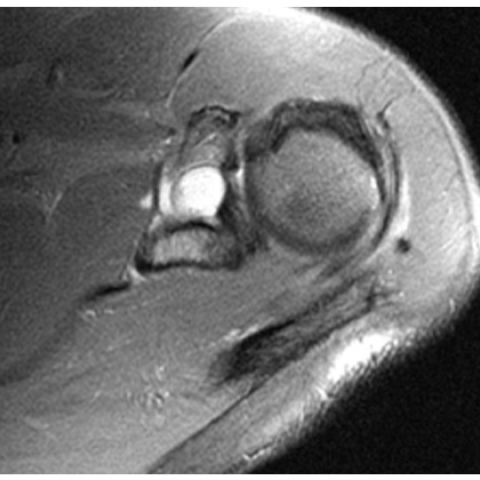
A well-defined cystic lesion seen in the suprascapular notch and spino-glenoid notch. The lesion appears T1 hypointense and hyperintense on T2. On postcontrast scan, the lesion shows peripheral enhancement with a central non-enhancing area.
Discussion
- Background: Supra-scapular nerve arises from the upper trunk of brachial plexus and is mainly supplied by C5, C6 and sometimes by C4. It has mixed sensory and motor supply. At the level of supra-scapular fossa, the nerve gives a motor branch to the supraspinatus and receives a sensory branch from the surrounding glenohumeral and acromioclavicular joint [1]. At the infraspinatus fossa, the nerve is purely motor with supply to infraspinatus muscle.
- Clinical Perspective: Supra-scapular nerve compression is uncommon and uncommonly diagnosed due to non-specific findings. The supra-scapular nerve is vulnerable to entrapment neuropathy at the supra-scapular notch and spino-glenoid notch to a narrow fibro-osseous tunnel. Various causes of compression include paralabral cyst, lipoma, haematoma, and malignant neoplasms [2, 3].
- Imaging Perspective: Diagnosis is based on the clinical features, electromyography findings, and imaging. MRI is the modality of choice in these cases. Compressive neuropathy presents with direct and indirect signs. The direct signs are related to nerve findings including abnormalities in size, position, and signal changes [4]. Indirect signs are related to nerve denervation. Acute denervation presents with hyperintensity of the involved muscles (supraspinatus and infraspinatus muscle) and chronic denervation presents with loss of muscle bulk and fatty infiltration. Ganglia appear hypo to isointense on T1, hyperintense on T2 and peripheral enhancement on post-contrast phase.
Ganglia can be treated by either arthroscopic approach or open repair for cyst decompression/excision and associated labral tears.
Differential Diagnosis List
Final Diagnosis
Suprascapular nerve entrapment secondary to ganglionic cyst
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Axial T2 fat saturated scan

Coronal T1-weighted scan

Coronal T2-weighted images


Sagittal T2 fat-saturated image


Post-contrast sagittal images


Sagittal T2 fat-saturated image

Coronal T1-weighted scan


1. Imaging Findings
Based on the provided shoulder MRI images (including T1, T2, and contrast-enhanced sequences), there is a well-defined, roughly round cystic signal lesion near the supraspinatus and infraspinatus tendon area in the posteriosuperior aspect of the shoulder joint. On T1-weighted images, it appears as relatively low or isointense signal, and on T2-weighted images, it shows high signal, consistent with joint cavity or synovial fluid-like lesions (e.g., joint cyst, tendon sheath cyst, or synovial cyst). The lesion is located in the posteriosuperior region of the glenoid or between the scapular spine and the glenoid, potentially compressing or stretching the suprascapular nerve. No obvious bony destruction or significant joint structural abnormality is observed, but some alterations in local muscle density or fiber orientation may suggest the need to watch for muscle atrophy or abnormal signals (especially in the supraspinatus and infraspinatus muscles).
2. Potential Diagnoses
-
Suprascapular Nerve Compression Neuropathy:
In this case, the patient presents with left upper limb weakness, particularly noticeable during shoulder abduction, external rotation, or lifting heavy objects. The MRI shows a cystic lesion near the suprascapular notch or spinoglenoid notch, suggesting that the nerve passing through these fibrous-osseous channels may be compressed. The suprascapular nerve primarily innervates the supraspinatus and infraspinatus muscles; compression can lead to decreased muscle strength and restricted movements. The lack of significant sensory deficits also aligns with the feature that the suprascapular nerve provides mainly motor innervation in the region of the infraspinatus.
-
Rotator Cuff Pathology or Tendon Tear:
Rotator cuff tendinopathy or partial tendon tears can also cause shoulder weakness, often accompanied by pain, impingement signs during joint movement, and even night pain. If the MRI shows only a cystic lesion without obvious tendon disruption or signal interruption, the likelihood of a major rotator cuff tear is relatively low. However, it is still important to consider possible concurrent rotator cuff degeneration or overuse injury.
-
Other Neurogenic Lesions or Masses:
Such as humeral head-related cysts, lipomas, or other benign or malignant tumors. If the cystic lesion is located near the shoulder joint and the labrum, a paralabral cyst (resulting from a labral tear with fluid leakage) should also be considered. However, in conjunction with clinical presentation, the most common and fitting scenario remains a tendon sheath/synovial cyst leading to suprascapular nerve compression.
3. Final Diagnosis
Considering the patient’s age (31 years old), the absence of significant sensory abnormalities, the primary complaint of unilateral upper limb weakness, and an MRI finding of a cystic lesion in the region where the suprascapular nerve travels, the most likely diagnosis is:
Compression neuropathy of the suprascapular nerve (in the infraspinatus region), presumably caused by a joint cyst or synovial cyst.
If uncertainty remains, an electromyography (EMG) could help confirm nerve conduction impairment, or a repeat MRI could be performed to assess any changes in the size or shape of the cyst. If necessary, aspiration or surgical exploration may be warranted for a definitive diagnosis.
4. Treatment Plan and Rehabilitation
-
Conservative Treatment:
- For mild symptoms and in cases where muscle strength has not significantly declined, an initial conservative approach may be taken. This may include appropriate rest and reducing frequent or excessive shoulder abduction and external rotation.
- Physical therapy and rehabilitation: Under the guidance of a professional therapist, adjust posture, strengthen surrounding shoulder muscles, and perform joint mobilization and stretching. Non-steroidal anti-inflammatory drugs (NSAIDs) may be used to alleviate local inflammation and pain.
-
Surgical Intervention:
- If the cyst is large or clearly compressing the nerve and causing persistent muscular weakness, arthroscopic or open surgery for cyst resection or drainage may be considered, along with any necessary labral repair.
- Postoperatively, strengthen shoulder joint function training to prevent adhesions and recurrence.
-
Rehabilitation / Exercise Prescription Recommendations (FITT-VP Principle):
- Frequency (F): 3 to 5 sessions of rehabilitation and functional training per week, adjusted according to individual tolerance.
- Intensity (I): Begin with low intensity, avoiding significant pain or persistent soreness. Gradually increase resistance over time, such as using resistance bands or light dumbbells.
- Time (T): 20–30 minutes per session, including warm-up and cool-down. After each session, consider applying ice or physiotherapy.
- Type (T): Focus on exercises that enhance shoulder stability and muscle strength, such as seated external rotation, bent-over rowing, and isometric exercises around the shoulder. Core stability exercises should also be incorporated.
- Progression (P): Once there is marked improvement in muscle strength and range of motion, progressively increase the complexity and resistance of exercises—for example, gradually increasing the angle of external rotation or introducing resistance training. Continuously monitor improvements in muscle strength and joint mobility.
Throughout the rehabilitation process, carefully observe comfort in the shoulder joint and scapular region. If any exercise causes significant pain or instability in the shoulder, promptly adjust or discontinue that exercise.
Disclaimer: This report is intended only as a reference based on existing clinical and imaging information and does not replace in-person consultation or professional medical advice. If you have any further questions, please seek medical attention or consult an orthopedic/sports medicine specialist.
Human Doctor Final Diagnosis
Suprascapular nerve entrapment secondary to ganglionic cyst