Multifocal epithelioid haemangioendothelioma



Clinical History
A 41-year-old man presented with a painful mass in the left leg. As an antecedent of interest, he had had a fracture of the left tibia and fibula 15 years before, which was treated surgically.
Imaging Findings
An X-ray, a CT scan and a MRI of the leg were performed and a US-guided biopsy (Fig. 3) to confirm the diagnosis. It was completed with a thoracoabdominal CT.
The radiograph and CT showed an osteosynthesis material in relation with spiroid fracture and an osteolytic lesion involving the anterior aspect of the tibia with cortical breakthrough and soft-tissue mass. No periosteal reaction or mineralised matrix were seen. The tumour presented calcified trabeculae in its interior with "soap bubble" appearance (Fig. 1 and 2).
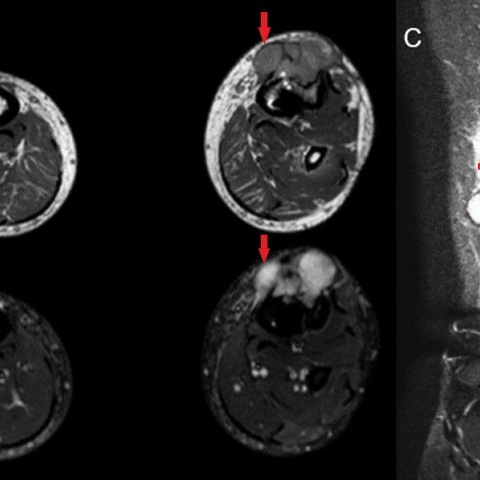
MRI shows marked extension of the tumour to the soft tissues with lobed contours and a homogeneous signal, except for septa (Fig. 4). The tumour was biopsied and the results were: malignant neoplasic proliferation constituted by epithelial cells with immunohistochemical markers compatible with epithelioid hemangioendothelioma (Fig. 5). It was completed with a thoracoabdominal CT that showed another similar lesion in the left iliac bone (Fig. 6).
Discussion
Malignant vascular tumours of the bone are rare, <1% of primary malignant bone tumours.
The epithelioid haemangioendothelioma (EHE) is a vascular tumour of intermediate-grade malignancy between haemangioma and angiosarcoma in terms of frequent local recurrences and metastatic potential [1, 2]. Weiss et al. described it first in 1982 as a vascular neoplasm of both bone and soft tissue [3]. In bones, EHE is located in metadiaphyseal, or less commonly, epiphyseal region of the lower extremities [2, 3, 4]. It can occur at almost any age (especially in the 2-3nd decade) with a slight male predominance [4]. Generally, patients complain of pain and swelling in the affected area. In 50% of cases multifocal disease is seen (multiple lesions in a single bone or multiple bone involvement).
Radiography typically reveals a cortical or medular expansive lytic lesion without matrix mineralisation. Calcification is infrequent, and periosteal reaction is rare in the absence of pathologic fracture. Cortical disruption, soft tissues and joint invasion can be present. [2] The "soap bubble" appearance has been described [5].
In MRI, EH has low to intermediate signal on T1-weighted images and high signal on T2-weighted-images with homogeneous enhancement after the injection of gadolinium [2].
The first diagnoses were adamantinoma and osteofibrous dysplasia. Soft tissue mass didn't allow us to rule out malignancy, and another similar lesion led us to consider metastasis and myeloma in a patient older than 40 years of age.
Although, before the multiplicity of bone lesions, absence of periosteal reaction and soft tissue mass the radiologist must include vascular tumours in their diagnoses. It is essential to suspect a vascular tumour, so that the pathologist can include vascular specific markers of endothelial cells (CD31, CD34, factor-VIII). [5]
It is important to know the 4th edition of the World Classification of Tumors of Bones and Soft Tissues of the WHO (2013). It includes genetic characterisation of EHE (for example, has been reported that YAP1-TFE3 translocation defines a subset which tend to affect younger adults and t(1;3)(p36;q23–25) is present in EHE at all anatomical sites) and proposes risk stratification according to size and mitotic activity [6].
EHE has a variable clinical course, usually prolonged. In some publications, the multifocal disease was thought to have a better prognosis. However, in the largest series, the overall survival for solitary disease was reported as 89% compared with 50% in multifocal disease.
Complete surgical excision is the treatment of choice. Others: preoperative embolisation, radiofrequency ablation and radiotherapy (alone or in conjunction with surgery). [2, 3]
Differential Diagnosis List
Final Diagnosis
Multifocal epithelioid hemangioendothelioma.
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Anteroposterior (A) and lateral (B) radiograph of left leg

Volume rendering image

MRI of the legs
Histology

Axial nonenhanced CT scan of the pelvis.

US guided biopsy

Medical Imaging Analysis Report
I. Imaging Findings
Based on the patient’s history of left lower leg fracture fixation (visible intramedullary nail and fixation plate), on X-ray plain films and CT reconstruction images, multiple lytic lesions can be observed in the cortex and medullary cavity of the mid-distal tibia. They have relatively irregular margins, with partial cortical expansion. A “soap-bubble-like” appearance is noted in some areas. Although there is partial cortical destruction, no significant extensive periosteal reaction is evident. On MRI, T1-weighted images show predominantly medium to low signal intensity, T2-weighted images show high signal intensity, and the lesions are markedly enhanced after contrast administration, suggesting rich blood supply. In the adjacent soft tissue, a local mass can be observed, indicating certain soft tissue involvement.
II. Potential Diagnoses
Taking into account the patient’s age, clinical presentation of left lower leg pain and swelling, and the radiological findings of lytic and vascular characteristics, the following are considered as key differential diagnoses:
- 1. Vascular tumor (especially endothelial origin): Given the imaging and pathological features hinting at a vascular tumor, including hemangioma, angiosarcoma, or moderately malignant epithelioid hemangioendothelioma (EHE).
- 2. Adamantinoma: Commonly occurs on the anterior cortical surface of the tibia and may present as a lytic lesion, but its pathology does not align closely with a vascular tumor.
- 3. Fibrous bone lesions (e.g., fibrous dysplasia, ossifying fibroma): Some cases may show expansile lytic destruction, but these lesions typically do not exhibit a pronounced vascular enhancement pattern.
- 4. Metastatic lesions or multiple myeloma: In patients over 40 years old with multiple lytic foci, metastasis or myeloma should be considered. However, absence of notable systemic symptoms or laboratory abnormalities may reduce this likelihood.
III. Final Diagnosis
Combining the imaging characteristics (multiple lytic lesions with marked enhancement, lacking significant periosteal reaction, with local soft tissue masses) and pathology results indicating positivity for endothelial markers (CD31, CD34, etc.), the most likely diagnosis is “Epithelioid Hemangioendothelioma (EHE)”. This is a moderately malignant vascular tumor that shows local aggressiveness and potential for metastasis. Further confirmation of lesion extent and treatment strategy requires correlation with clinical symptoms, laboratory testing, and follow-up imaging.
IV. Treatment Plan and Rehabilitation
The core management strategy, based on the current diagnosis and patient’s condition, involves surgical excision or lesion clearance, with additional local treatments considered if needed. Recommendations are as follows:
- Surgical Strategy: For solitary lesions or resectable multifocal lesions, aim for complete lesion clearance or wide resection. Combine with internal fixation or reconstructions as needed to maintain limb stability.
- Other Treatments: Preoperative vascular embolization can be considered to reduce intraoperative bleeding. In certain cases, radiofrequency ablation or radiotherapy may be selected.
- Postoperative Rehabilitation and Exercise Prescription (FITT-VP Principle):
- Frequency: Initially 2–3 rehabilitation sessions per week, gradually increasing to 3–5 sessions per week.
- Intensity: Begin with low-intensity joint mobility and muscle strengthening exercises (e.g., straight leg raises, ankle pump exercises). Progress to moderate-resistance training, ensuring pain or excessive fatigue is avoided.
- Time: Start each session with about 10–15 minutes, gradually increasing to 20–30 minutes as tolerated.
- Type: Early focus on range of motion exercises and isometric muscle contractions, incorporating water therapy or assistive devices gradually. Later stages may include aerobic activities (e.g., cycling, swimming) and weight-bearing exercises for the lower limbs.
- Progression: Increase exercise intensity and duration as pain subsides and bone and soft tissue recover. Avoid premature heavy weight-bearing or pivoting movements.
- Volume & Individualization: Tailor exercise type and volume according to pain level, flexibility, bone quality, and cardiopulmonary function. Periodic imaging follow-ups are required to monitor lesion status and prevent progression or fractures.
- Special Considerations: If the patient has brittle bones or potential multisite lesions, extra precautions and monitoring are necessary to reduce the risk of falls or overtraining. Regularly review imaging and laboratory tests to assess local tumor control and overall health status.
V. Disclaimer
This report is based solely on the patient’s current medical history and radiological data, serving as a reference and not as a substitute for in-person consultations or licensed medical advice. Specific treatment plans require integration of clinical examinations, histopathological findings, and the attending physician’s assessment. Please consult a medical professional promptly if any doubts or changes in symptoms arise.
Human Doctor Final Diagnosis
Multifocal epithelioid hemangioendothelioma.