


A 14-year-old boy came to the emergency department with chief complaints of sudden onset of left hip pain for 1 month associated with high-grade fever. There was no significant past medical history. On examination, the patient’s hip was placed in external rotation, abduction and mild flexion position.
Plain radiograph of pelvis with both hips shows destruction of articular surface of the head of the left femur and acetabulum with cortical irregularity, juxtaarticular osteopenia, joint space widening, reduction in volume of femur head with its mild supero-lateral dislocation. (Fig. 1).
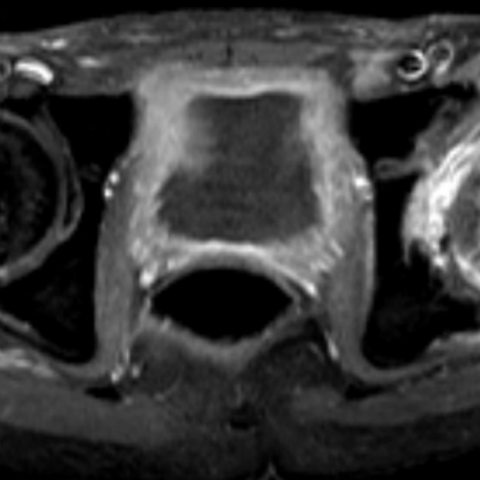
On magnetic resonance imaging, diffuse marrow oedema is noted within the left femoral head, neck, proximal meta-diaphysis (Fig. 2a). Linear hypointensity (hypointense on all pulse sequences) is noted involving proximal meta-diaphysis of left femur suggestive of dead bone/sequestrum (Fig. 2b, c).
Marrow oedema is noted involving the left acetabulum (Fig. 2a).
Destruction of the head of the left femur and adjacent acetabulum with resultant mild superolateral dislocation of the femoral head is noted (Figure 2a, b, c).
Mild left hip joint effusion, intensely enhancing synovial thickening is noted (Fig. 2, 3).
Peripherally enhancing collection is noted anterior to left hip joint (Fig. 4).
Soft tissue oedema is noted involving left pyriformis, vastus lateralis, gluteus medius and minimus (Fig. 5).
Acute osteomyelitis is an acute (<2 weeks) infection of bone, its incidence in developed countries being 8-10/10,000 and up to 80/10,000 in developing countries. The incidence of septic arthritis is half of the incidence of osteomyelitis [2].
The most common causative organism is Staphylococcus aureus and the most common mode of infection is via the haematogenous route [1].
Septic arthritis is a well known complication of acute haematogeneous ostemyelitis. However, primary infection can originally affect the joint, then penetrate the epiphyseal cartilage, and finally spread into the metaphyseal region through transphyseal vessels present only in the first 12/18 months of life [5].
Chief complaints include irritability, limping, localised pain in the anterior aspect of the hip joint, often radiating towards the knee [3].
Neutrophilic leucocytosis, raised C reactive protein and ESR are common laboratory findings [3].
Early radiographic findings include soft tissue swelling, joint space widening, periarticular osteopenia, blurring of adjacent fat planes. Late findings include joint space narrowing, articular surface irregularity, erosions, subluxations and dislocations [1, 3]. Associated osteomyelitis will additionally show cortical fissuring and elevation of periosteum in early phase. Late findings include lamellated periosteal reaction, sequestrum and cloaca with adjacent osteopenia [1].
Ultrasound will detect even 1 mm of joint effusion. Capsular distension with capsule to bone distance difference of >=2 mm as compared to opposite side is significant. Internal echoes point more towards septic effusion in absence of trauma, whereas anechoic fluid goes more in favour of transient synovitis [3].
Magnetic resonance imaging has proved to be a problem-solving tool and helps in diagnosing septic arthritis as early as 24 hours after onset of infection [4]. The sensitivity and specificity of gadopentetate dimeglumine for diagnosing septic arthritis is 100% and 77% respectively [4]. MRI findings include joint effusion, synovial thickening, fairly intense synovial enhancement. Dynamic contrast enhancement may distinguish the early enhancing synovium from delayed enhancing joint fluid [4]. Associated articular cartilage destruction, subchondral bone erosion, dislocations, soft tissue oedema, soft tissue abscess with rim enhancement are also noted. Associated osteomyelitis can easily be detected by MRI as altered signal intensity marrow oedema, intraosseous abscesses, sequestra, cloaca, lamellated periosteal reaction [4].
Triple phase bone scan using technetium 99m labelled methylene diphosphate used in detection of multifocal disease [2].
Take home message: Early diagnosis of septic arthritis is utmost important. Any delay in diagnosis may increase morbidity and lead to complications such as bone and cartilage destruction, osteonecrosis, secondary osteoarthritis, osteomyelitis, and eventually ankylosis.
Osteomyelitis of femur complicating as septic arthritis of hip
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.









Based on the provided anteroposterior (AP) pelvic X-ray and MRI images, the following major features are observed:
Based on the above imaging findings and the patient’s clinical history (14-year-old boy with acute left hip pain and high fever for one month), the following diagnoses should be considered:
Taking into account the patient’s age, acute onset, high fever, likely elevated white blood cells and inflammatory markers (if known), and significant synovial thickening, effusion, bone marrow edema, and purulent changes in soft tissue on MRI, the most probable diagnosis is:
If there are still questions regarding the diagnosis, further confirmation through joint aspiration (obtaining joint fluid for bacterial culture) or bone biopsy if necessary is recommended.
1. Treatment Strategy
2. Rehabilitation/Exercise Prescription Suggestions
Once the joint inflammation and local infection are under basic control, a stepwise rehabilitation regimen can be initiated, following the FITT-VP principle:
Sample training routine (after inflammation subsides):
Disclaimer: This report is for medical information reference only and does not replace an in-person consultation or professional medical advice. If you have any questions or your condition changes, please seek medical attention promptly.
Osteomyelitis of femur complicating as septic arthritis of hip