Benign post-traumatic cortical cyst-like lesion following a distal radial fracture in a child



Clinical History
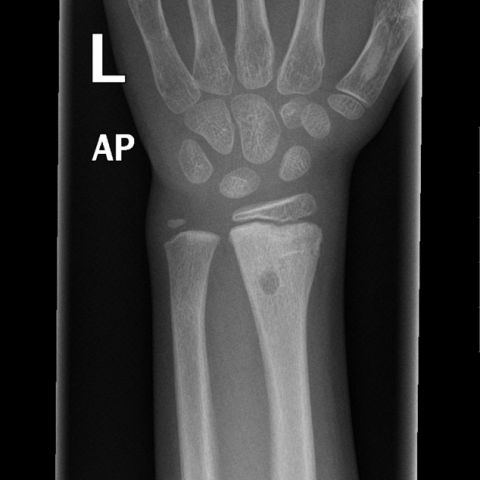
A 7-year-old girl fell on her left wrist and was diagnosed with a buckle fracture of the radius. Four weeks later there was a second trauma and re-fracture of the left distal radius was diagnosed.
Imaging Findings
The initial radiograph showed a buckle fracture of the distal radius. The radiograph made after the second trauma demonstrated a fracture of the left distal radius with some periosteal reaction, and proximal of the fracture in the dorsal cortex a well-defined oval-shaped lucency. Over time, radiographs showed more demarcation of the lucency, with a discrete partially sclerotic margin, and diaphyseal migration. MRI demonstrated a small cortical lesion, on the dorsal surface of the distal radius, without periosteal reaction or bone marrow oedema. The lesion showed high signal intensity on the T1-, T2- and T2-weighted images with fat suppression, with an adjacent thin rim of low signal intensity on all sequences, corresponding with the discrete sclerosis on the conventional radiographs. On the dynamic images during contrast administration the lesion showed minimal rim enhancement. The lesion measured 3 x 3 x 5 mm (LR x AP x CC).
Discussion
Since 1969, only 36 cases of post-traumatic cyst-like lesions in children have been reported in the medical literature. [1-7, 10] Other names used for these lesions are transient post-traumatic cortical defects, post-traumatic lipid inclusions, post-fracture subperiosteal cyst-like defects, post-fracture paediatric cyst and cyst-like cortical defects. [2, 6, 7, 10] The mean age at which these lesions occur is between 6, 5-7, 5 years (range 18 months - 15 years). [2-10] Approximately 90% of these lesions are located in the distal radius and are more often seen after greenstick and buckle fractures. [1-4, 7-10] They develop between four weeks to three months after the fracture. [2-7, 9, 10] They have also been described as an incidental finding during imaging after re-injury. [8, 9] They develop adjacent or proximal to the previous fracture site, within the area of periosteal reaction. [3-5, 7-10] Typically, the lesion is well-defined, round or oval-shaped, without surrounding sclerosis, and smaller than 10 mm. [1-9] Usually they are solitary, but can be multiple. [2-5, 8, 10] The lesion tends to migrate in the direction of the diaphysis with growth and will resolve spontaneously, normally between 6 months and 3 years. [2, 3, 5, 6] This lesion is benign, asymptomatic and needs no long-term follow-up. [1-10]
The aetiology of this lesion remains controversial. The fat-inclusion theory is the most accepted one and was described in 1990 by Malghem. It describes the transcortical leakage of intra-medullary fat in the subperiosteal haematoma, after a fracture of the distal radius, in which the periosteum remains intact and is only detached from the bone. [10] The theory of Philipps and Keats is based on subperiosteal haemorrhage that will calcify or resorb. [11]
Normally on MRI the signal intensity of the lesion is consistent with adipose tissue on all sequences. There is no surrounding bone marrow oedema. After contrast administration, the lesion does not enhance. [6] Usually these lesions have a low signal intensity on T2-weighted fat-suppressed images, diagnostic for a lipomatous content. In this specific case the signal intensity on T2-weighted images with fat suppression was high, indicating absence of fat inclusion. Likely the high signal intensity on all sequences is due to haemorrhage. Because of these signal intensities we should, therefore, consider the possibility that the cortical cyst-like lesion is the same entity as a post-traumatic subperiosteal haematoma and can develop with or without fat inclusion.
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Post-traumatic cortical cyst-like lesion due to haemorraghe following a distal radial fracture in a child
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Radiograps of the left wrist after first trauma


Radiograps of the left wrist after second trauma


Follow-up 6 weeks after second trauma

Follow-up 4.5 months after the second trauma


MRI performed 5 months after second trauma






Medical Imaging Analysis Report
I. Radiological Findings
The patient is a 7-year-old girl who sustained a compressive (buckle) fracture of the left distal radius 4 weeks ago due to a fall. Subsequently, she experienced another trauma, and follow-up imaging studies were performed. The main findings are as follows:
- X-ray (AP and lateral views): Changes consistent with fracture healing are observed in the distal left radius. The local cortical bone is slightly thicker than previously noted, and a focal radiolucent area can be seen in the original fracture site or in the subcortical region proximally. This area appears round or oval, with clear boundaries and no obvious sclerotic rim. A new fracture line may have appeared following the repeated trauma, but overall alignment and apposition remain acceptable.
- MRI (T1, T2, and fat-suppression sequences, etc.): A cystic signal lesion is visible near the cortical bone of the distal radius. Certain sequences display high signal intensity, suggesting that its content could be hematic or fluid in nature. There is no evident bone marrow edema signal, no marked soft tissue swelling, and no destructive changes to the surrounding cortex. No substantive enhancement is seen after contrast administration.
In summary, a small cyst-like lucent lesion is found in the cortical (or subperiosteal) region of the distal radius, consistent with descriptions of the “post-traumatic cyst-like lesion.”
II. Potential Diagnoses
Based on the patient’s history (two traumas), age, and imaging features, the following diagnoses or differential diagnoses may be considered:
- Post-traumatic cyst-like lesion
- Characteristics: Often found in children following greenstick or compression fractures of the distal radius. A cyst-like area forms in the subcortical region, with imaging signals or densities potentially displaying fat or hematic components.
- Mechanism: Possibly related to fatty marrow or a subperiosteal hematoma that migrates through the fracture line, eventually resolving spontaneously.
- Simple bone cyst
- Characteristics: Commonly occurs in the metaphysis of long bones in adolescents, usually in the proximal humerus or proximal femur. Distal radius involvement is less common.
- Not typical in this case: Its location, clinical history, and imaging features are more consistent with post-traumatic changes.
- Aneurysmal bone cyst
- Characteristics: Typically shows septations, expansile remodeling, and potential cortical erosion. MRI commonly reveals blood-filled septations.
- Not favored in this case: X-ray does not show obvious expansion or destructive changes.
- Subperiosteal hematoma or a rare infectious process
- If it is a subperiosteal hematoma, it could coexist or be confused with a post-traumatic cyst-like lesion.
- Infection (e.g., subperiosteal abscess) typically presents with pain, inflammation, and signs of bone destruction, which do not match the imaging or clinical presentation in this case.
III. Final Diagnosis
Based on the imaging findings, the history of repeated trauma, and the common post-traumatic cystic changes seen in the distal radius among children, the most likely diagnosis is:
“Post-traumatic cyst-like lesion”.
Because this entity is generally benign, asymptomatic, and tends to resolve spontaneously, no special intervention is usually required.
IV. Treatment Plan and Rehabilitation
- Treatment Strategy
- For the post-traumatic cyst-like lesion itself, observation and follow-up are usually sufficient, without the need for surgery or other unnecessary interventions.
- If there is a concurrent distal radius fracture, management includes cast or splint immobilization depending on the degree of displacement, ensuring proper alignment and healing.
- If the cystic lesion continues to enlarge or poses a risk to bone strength (which is rare), further evaluation and consultation with a specialist may be warranted.
- Rehabilitation/Exercise Prescription (FITT-VP Principle)
After clinical fracture healing is confirmed and the lesion is deemed stable with no active progression or special risks, moderate limb functional training can be initiated:
- Frequency: 2–3 times per week initially, increasing to 3–4 times per week as tolerated.
- Intensity: Start with mild resistance or range-of-motion exercises. If no discomfort develops, gradually introduce resistance bands or light dumbbells (1–2 kg) for gentle strength training.
- Time: 15–20 minutes per session, progressing gradually to 30 minutes.
- Type: Exercises include range-of-motion training for the wrist and forearm (flexion, extension, pronation, and supination) and light grip strength exercises. Daily activities can also be gradually increased.
- Progression: Increase load based on pain relief and functional recovery. If pain or swelling occurs, postpone exercises and re-evaluate.
- Volume & Individuality: The specific exercise program should be flexibly adjusted according to the child’s tolerance and the status of bone healing, ensuring safety and avoiding re-injury.
It is recommended to train under the guidance of a rehabilitation or orthopedic specialist. Seek medical advice promptly if any abnormal pain or discomfort arises.
Disclaimer
This report is based on current imaging and clinical history and is for reference only. It does not replace an in-person consultation or professional medical advice. If any further concerns or changes in condition occur, please consult a specialist or visit a medical facility promptly.
Human Doctor Final Diagnosis
Post-traumatic cortical cyst-like lesion due to haemorraghe following a distal radial fracture in a child