Diastematomyelia



Clinical History
The patient presented with abdominal pain, changed stool colour, vomiting and tiredness. At clinical examination a mass was found in the upper abdomen. The patient had no neurological symptoms.
Imaging Findings
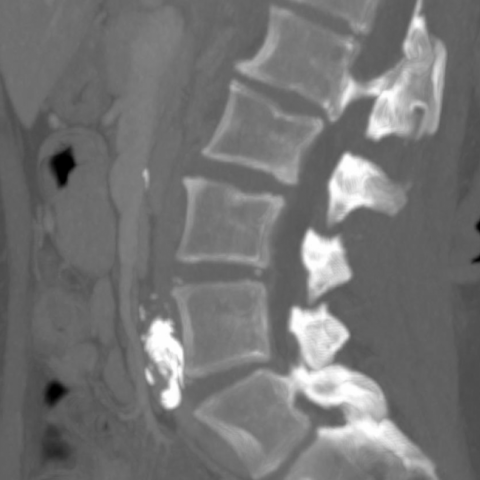
Contrast-enhanced CT of the chest and abdomen was performed as a malignant disease was suspected. The scanning showed enlarged liver with diffuse parenchymal changes in keeping with possible acute hepatitis. As an incidental finding a sagittal osseous septum through the spinal canal at the L1-level was detected (Fig. 1-3). Additionally the L1 vertebra was found to have an enlarged spinosus processes with a central cleft (Fig. 3). No other abnormalities were seen in the spine and the diagnosis of diastematomyelia was made. Subsequent MRI performed to assess the liver changes confirmed the diagnosis of diastematomyelia (Fig. 4). No malignant disease was detected at CT or MRI. Acute viral hepatitis (CMV) was made by serology.
Discussion
Diastematomyelia is a rare congenital abnormality in which the spinal cord is split in two parts (often by a rigid osseous septum). Diastematomyelia accounts for approximately 4% of all congenital spinal abnormalities. It is the result of the fetus having an accessory neuroenteric canal which causes the spinal elements to form as two sets of structures [1]. The lumbar and thoracolumbar region is the most common site for diastematomyelia with 50% occurring between L1 and L3, and 25% occurring between T7 and T12 [2]. Two types of diastematomyelia have been described: Type 1 (classic diastematomyelia) with duplicated dural sac with a midline spur, and type 2 with a single dural sac. The deformity is often accompanied by segmental anomalies of the vertebrae [3].
Patients with diastematomyelia may present with neurological signs and symptoms, but some patients are asymptomatic. The symptoms have shown to be significantly higher in type 1 than in type 2 diastematomyelia [1]. Patients with type 2 may be minimally affected or entirely asymptomatic.
Symptomatic patients can present with neurologic deficits in the lower limbs and perineum; causing leg weakness, low back pain, muscular atrophy, reflex changes and incontinence. Associated abnormalities may be present including congenital scoliosis, foot deformities and characteristic changes of the dorsal skin.
Surgical treatment with extirpation of the osseous septum (and duralplasty) is recommended for type 1 diastematomyelia, whereas conservative treatment is recommended for asymptomatic type 1 and all cases of type 2 diastematomyelia [4, 5]. For symptomatic patients correct diagnosis is important for optimal management and treatment before progression of neurological deficit. The present case is a case of type 1 diastematomyelia. The patient was asymptomatic and conservative treatment was chosen. Cross-sectional imaging with CT and MRI are the best imaging modalities to diagnose diastematomyelia. The bony structures are best evaluated with CT whereas the spinal cord should be evaluated with MRI.
In conclusion, diastematomyelia is a rare abnormality of the spinal cord with typical imaging findings at CT and MRI.
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Diastematomyelia - type 1
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Axial CT

Axial MRI

Sagittal CT
Coronal CT

Imaging Findings
CT and MRI images reveal a pronounced splitting phenomenon of the spinal canal in the lumbar region, accompanied by a bony longitudinal septum, suggesting that the spinal cord is divided into two separate channels. A bony ridge or protrusion can be identified along the midline of the spinal canal, clearly separating the dura. Congenital morphological changes in the vertebral bodies are also noted.
CT distinctly illustrates the bony structures, allowing clear identification of the bony partition in both axial and reconstructed images. MRI demonstrates two separate neural structures at the site of the split, consistent with typical “split cord malformation” imaging features. Currently, there are no evident signs of nerve compression caused by an intraspinal occupying lesion.
Potential Diagnoses
- Congenital Diastematomyelia (Spinal Cord Split): This most closely aligns with the imaging findings described above, particularly the bony septum and the characteristic split in the spinal cord. Depending on whether there are two distinct dura (cord) sacs and a bony spur, it can be further categorized into Type 1 and Type 2.
- Other Forms of Congenital Spinal Dysraphism: For example, spina bifida or spinal lipoma may also exhibit abnormal spinal canal structures, but typically lack a distinct midline bony septum on imaging and are often accompanied by more apparent neurological symptoms.
- Other Intraspinal Space-Occupying or Partition Lesions: For instance, an intraspinal schwannoma or cyst can cause spinal cord displacement, but these lesions tend to be localized and do not produce a bony septum.
Final Diagnosis
Taking into account the imaging characteristics (bony septum dividing the spinal canal and split spinal cord) alongside the current absence of neurological symptoms, the most likely diagnosis is Type 1 Diastematomyelia. This type commonly involves a bony or fibrous septum that separates the dural sac, confirmable through comprehensive imaging studies. Because the patient does not present with significant neurological impairment at this time, conservative management is advised.
Treatment Plan and Rehabilitation Program
Treatment Strategy:
- Conservative Management: Given the patient currently has no neurological symptoms, regular follow-up is recommended, with continued monitoring of clinical signs and imaging findings. Should lower limb sensory changes, muscle weakness, or bladder/bowel dysfunction associated with nerve compression arise, further surgical interventions may be considered.
- Surgical Treatment: In cases of pronounced or progressive neurological compromise, surgery to remove the bony septum and perform dural repair (duralplasty) may be necessary. However, as this patient does not exhibit progressive neurological deficits, surgical indications are not compelling at present.
Rehabilitation / Exercise Prescription Recommendations:
- In the absence of neurological symptoms, engage in moderate core stability exercises (e.g., plank, supine bridge) to maintain lumbar and dorsal muscle strength and reduce spinal load.
- Gradually introduce low-impact aerobic activities (e.g., swimming, elliptical training, brisk walking) 3–5 times per week for 20–30 minutes each session. Intensity should be such that you experience slight breathlessness but can still converse normally.
- Once spinal alignment is stable, perform gentle lumbar and back stretching exercises daily (e.g., five-point support, cat-camel stretch) to maintain joint flexibility. Avoid high-intensity twisting or heavy lifting.
- If lower limb or back discomfort occurs, immediately reduce exercise intensity and consult a specialist or rehabilitation therapist.
- FITT-VP Principle: Adjust Frequency, Intensity, Time, and Type of exercise based on individual fitness levels, with periodic assessments for effectiveness and safety. Progress (P) appropriately over time.
Monitoring bone health is also essential. If subsequent checks indicate osteoporosis or compromised spinal stability, reduce high-impact weight-bearing exercises and undertake further evaluations.
Disclaimer: This report is a reference-based analysis derived from current imaging and clinical information. It should not replace in-person medical consultations or the guidance of a professional healthcare provider. If you have any questions or develop new symptoms, please consult a specialist as soon as possible.
Human Doctor Final Diagnosis
Diastematomyelia - type 1