


A 71-years-old female patient presented with an enlarging painful mass in the inner region of the left thigh. Physical examination revealed a palpable hard mass of about 5 cm, ostensibly adhered to the deep layer. There were no other relevant findings.
Ultrasound (US) images, including greyscale and colour Doppler, and magnetic resonance (MR) images were subsequently performed for further evaluation.
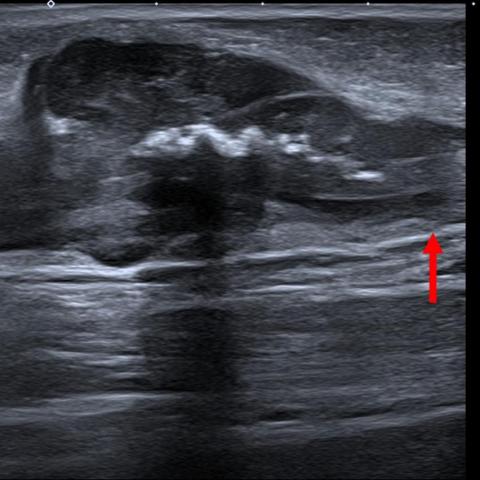
High-resolution greyscale US image (Fig. 1a) showed a solid soft-tissue mass located in the subcutaneous fat layer in contiguity with the great saphenous vein. Colour Doppler (Fig. 1b) detected scarce vascularity inside the lesion. The key finding is the mural thickening of the greater saphenous vein, which is encased by the mass. This finding reveals the intramural origin of the mass and the extra vascular extension.
MRI exhibits a well-circumscribed subcutaneous soft tissue mass, isointense to muscle on axial T1-weighted image and hyperintense on fat saturated DP-weighted image (Figs. 2a and 2b).
Sagittal and axial contrast-enhancement T1-weighted SPIR images (Figs. 2c and 2d) demonstrate mural thickening of the greater saphenous vein and eccentric location of the saphenous-dependent mass. Note the similar behaviour and intense enhancement of both, the mural vessel thickening and the adjacent mass.
Leiomyosarcoma (LMS) is a rare soft-tissue malignant tumour accounting for around 6% of all soft tissue sarcomas. Primary vascular location is extremely rare representing less than 2% of all LMS [1].
Vascular LMS develops from the smooth muscle cells of the vessel rising in veins five times more than in arteries [1]. It appears in vessels such as the inferior vena cava, great saphenous vein, femoral vein and popliteal vein, being the inferior vena cava, the most common vessel affected [2].
Vascular soft-tissue LMS frequently presents as an enlarging palpable mass. Other occasional symptoms are oedema and simulated thrombosis. In this context, US is the first test performed at our institution.
The diagnostic modality of choice is MRI since it allows the full assessment of the vessel’s involvement and permits the evaluation of the entire limb preoperatively.
The final diagnosis is reached by performing an image-guided core needle biopsy [3]. In our case we performed a US-guided core needle biopsy and the histological diagnosis was high-grade LMS.
Chest CT is mandatory to rule out metastasis and brain and abdominal CT may be added for staging [4].
The main treatment is surgical tumour and vascular segment affected excision with negative margins. The effectiveness of adjuvant therapies is unclear, further studies are needed. Radiotherapy permits a better local control of the disease without improvement on survival or recurrence-free survival [5]. In advanced stages chemotherapy must be considered [5].
Soft-tissue LMS are aggressive tumours with poor prognosis. They have the lowest rates of survival among all soft-tissue sarcomas. Vascular LMS have the worst prognosis of the soft-tissue LMS [5].
The differential diagnosis includes other soft tissues sarcomas, epithelioid haemangioendothelioma [6] and vascular leiomyoma. The latter usually measures less than 2 cm and does not demonstrate association with neurovascular structures unlike malignant lesions such as sarcomas [7].
Written informed patient consent for publication has been obtained.
High-grade leiomyosarcoma of the great saphenous vein
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.





Based on the provided ultrasound (Figures 1, 2) and MRI (Figures 3, 4, 5, 6) images, the following observations can be made:
Based on the patient’s imaging findings and clinical data, the following differential diagnoses are primarily considered:
Considering the patient's age (71 years), clinical presentation (progressive pain, palpable mass), imaging findings (deep vascular involvement and marked enhancement), and biopsy results (indicating a high-grade leiomyosarcoma), the most likely diagnosis is: High-grade vascular leiomyosarcoma (Leiomyosarcoma).
If there are remaining diagnostic uncertainties or a need to clarify tumor staging and differentiation, further whole-body CT or MRI evaluation can be conducted, in combination with pathological immunohistochemistry for a comprehensive diagnosis.
Limb function recovery should be tailored to the extent of surgery, postoperative wound healing, and the patient’s overall fitness level, following a gradual, individualized rehabilitation program:
Throughout rehabilitation, closely monitor the patient’s overall health status and changes in lower-limb function. Engage a physical therapist or rehabilitation specialist as needed for professional guidance.
Disclaimer: This report provides reference analysis based on current information and cannot replace in-person consultation or professional medical advice. Specific treatment and rehabilitation plans should be finalized by specialists or rehabilitation professionals according to the patient’s actual condition.
High-grade leiomyosarcoma of the great saphenous vein