Amyloidoma of the spine with pathologic fracture of the odontoid process



Clinical History
A 64-year-old male with personal antecedents of light chain multiple myeloma and AL amyloidosis with good response to Daratumumab. The patient comes to haematologic consult for revision and refers neck pain of 5 days of evolution. He had no previous trauma or neurologic symptoms.
Imaging Findings
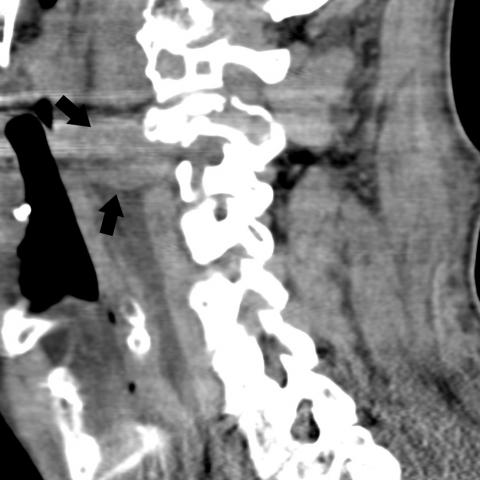
Cervical X-ray shows a pathologic fracture of the odontoid process. Cervical CT confirms the fracture and identifies the lytic lesion that affects the anterior arc of C1, the lateral mass of C1 and C2 and the odontoid process. Also a high-attenuation soft tissue component is visible that extends to the epidural space and especially to the prevertebral soft tissues. MRI shows a lobulated mass that affects anterior arc and lateral masses of C1, odontoid process, body and lateral masses of C2 with an important component of prevertebral soft tissue. Remarkably, it is very hypointense on T2 and STIR sequences and shows weak peripherical enhancement after the administration of Gd.
Discussion
In an elderly patient, any pathologic fracture that affects the spine should raise suspicion for metastatic involvement, multiple myeloma or plasmacytoma. However, in this patient, affected for multiple myeloma and light-chain amyloidosis, the presence of an amyloidoma should be considered. Amyloidosis is an unusual pathology (incidence of 6-10 cases/100.000 population) caused for abnormal deposition of insoluble proteins in different parts of the organism [1]. The most uncommon manifestation is the presence of pseudotumoral lesions with aggressive growing called amyloidomas [2]. They are more frequent in patients with systemic amyloidosis and multiple myeloma. Although we refer primaraily to solitary amyloidomas of the spine [3]. Amyloidomas of the spine produces symptoms depending on the location, size and compression of neurologic structures. Imaging techniques (CT and MRI) are useful for evaluation of the compression, for detecting complications such as fracture and planning surgery, either for fixation or biopsy, which is required for definitive diagnosis [4]. On conventional radiography and CT, we can see lytic lesions with variable grades of calcification and with tendency to extend to the soft tissues. Sometimes it can be heavily calcified mimicking osteogenic sarcoma, chondrosarcoma or calcified metastases [5]. MRI findings are more suggestive for diagnosis, although not pathognomonic. MRI findings consist of low-signal on T1WI and very low signal on T2WI with a variable enhancement, usually weak [6]. 18F-FDG PET has been considered a reliable method for the detection of active multiple myeloma; however, evidence of its diagnostic power in amyloidosis remains lacking [7]. Localised amyloidosis tends to show mild-to-moderate increased FDG uptake, similar to multiple myeloma and plasmocytoma. Besides, the molecular mechanism for 18F-FDG uptake remains speculative and probably related to inflammatory changes associated [8]. In this case, considering the instability of the fracture, an occipitocervical fixation was performed. During surgery, samples of bone and soft tissue were obtained for pathological analysis. Congo red staining and green apple birefringence confirmed the presence of extensive amyloid deposition. Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Cervical amyloidoma causing pathologic fracture of C2
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures










Imaging Findings
The patient is 64 years old with a known history of light chain type multiple myeloma and AL-type amyloidosis. This admission is due to neck pain, and imaging studies include cervical spine X-ray, CT, and MRI. The overall findings are as follows:
- X-ray: Shows instability in the upper cervical spine (especially the atlantoaxial region), with possible structural defects of the vertebral body or arch, suggesting a potential pathological fracture.
- CT scan: Reveals lytic lesions in the atlas and axis, accompanied by local bone destruction and fragmentation. Some areas show calcification or sclerosis. The lesion extends into the surrounding soft tissue, with increased density in the paravertebral soft tissue.
- MRI: On T1WI, the lesion appears with low signal intensity; on T2WI, the signal is also low or very low. After contrast administration, there is mild to moderate heterogeneous enhancement. The lesion involves the atlantoaxial joints and is associated with local soft tissue swelling, potentially compressing adjacent structures.
Potential Diagnoses
Considering the patient's age, history of light chain type multiple myeloma, and amyloidosis, the following differential diagnoses should be considered for the above-mentioned cervical spine lytic lesions:
- Relapsed or Progressive Multiple Myeloma/Plasmacytoma: Multiple myeloma can involve vertebral bodies or paravertebral bone with lytic changes and can lead to pathological fractures.
- Metastatic Lesions: In elderly patients, any pathological fracture in the spine necessitates ruling out metastatic disease, even if another known primary tumor already exists.
- Amyloidoma: Given the patient’s AL-type amyloidosis, an amyloidoma (pseudotumoral lesion) within the vertebra can cause local bone destruction, calcification, and soft tissue invasion. Imaging may show lytic changes with low signal intensity.
Final Diagnosis
Based on the patient’s history of light chain type multiple myeloma and AL-type amyloidosis, the characteristic imaging findings in the cervical spine (including lytic destruction, local calcification, low MRI signal, and mild enhancement), together with surgical pathology confirmation, the most likely diagnosis is:
Cervical Spine Amyloidoma (Pseudotumor) with Pathological Fracture
Surgical fixation and biopsy were performed in this case; Congo red staining observed under polarized light showed apple-green birefringence, confirming extensive amyloid deposition, thus establishing the diagnosis of an amyloidoma resulting in a pathological fracture.
Treatment Plan and Rehabilitation
Considering the patient’s age, bone condition, and extent of the lesion, a multidisciplinary approach is needed:
- Surgical Treatment: For unstable cervical spine lesions or those with nerve compression, occipitocervical or atlantoaxial fixation can be performed; decompression surgery may be necessary if indicated.
- Medical Treatment: For patients with concurrent amyloidosis and multiple myeloma, further intensified anti-myeloma therapy and management of amyloidosis (e.g., continuous targeted therapy, immunotherapy) may help control the disease.
- Rehabilitation and Exercise Prescription:
- Early Rehabilitation Stage (Postoperative 4-6 Weeks): Primarily use cervical collars or other external fixation devices to stabilize the neck and perform passive movements. Avoid excessive rotation or flexion-extension of the cervical spine. Light shoulder and upper limb activities may be undertaken to promote blood circulation and muscle recovery.
- Stabilization Stage (Postoperative 6-12 Weeks): Under the guidance of professional rehabilitation therapists, gradually introduce isometric neck exercises to progressively restore cervical range of motion. Low-intensity, short-duration neck muscle strengthening exercises may be employed (e.g., supine neck bridging for 5-10 seconds each time, 2-3 sets per day).
- Functional Reconstruction Stage (3 Months or More Postoperatively): Once bone healing is stable, introduce aerobic exercises such as walking on level ground or foam roller myofascial release, 3-5 times per week, 20-30 minutes each session. Gradually increase the duration and intensity, while closely monitoring cervical stability.
- FITT-VP Principle: Adjust the Frequency, Intensity, Time, and Type of exercise progressively based on the rehabilitation stage and patient tolerance (Progression), taking into account the surgical range and bone quality.
Precautions: Since the patient has multiple myeloma and fragile bones, avoid vigorous neck twisting or high-impact activities. Regular imaging and laboratory follow-up are necessary to monitor disease progression.
Disclaimer
This report is a reference analysis based on current imaging and clinical information. It does not replace an in-person consultation or professional medical advice. The patient should continue to follow the guidance of specialized clinicians based on their actual condition.
Human Doctor Final Diagnosis
Cervical amyloidoma causing pathologic fracture of C2