Atlantoaxial subluxation



Clinical History
A 10-years old girl with 3 months history of neck pain and stiffness experienced sudden worsening of symptoms with severe neck pain, headache, nausea with vomiting and dizziness. A clinical examination revealed torticollis with limited head rotation to the left, multiple reactive lymph nodes and subfebrile (37,5°C) body temperature.
Imaging Findings
US findings included multiple bilateral reactive lymph nodes and contracted sternocleidomastoid muscle (fig. 1).
Radiographs (fig. 2a, 2b) revealed signs of upper cervical vertebra rotation with no visible atlantoaxial subluxation (AAS).
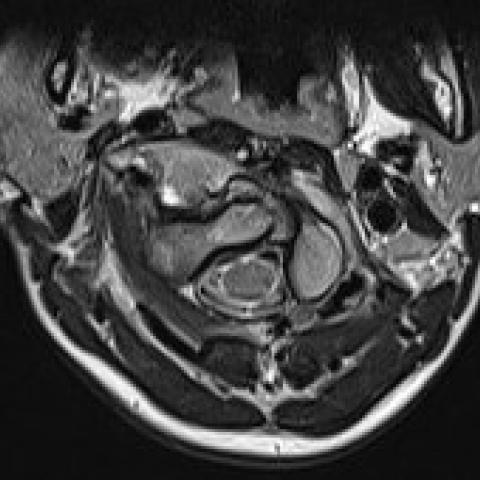
On MR imaging C1 to C2 subluxation of 70° was observed, with preserved transverse ligaments (fig. 3). Atlantodental interval (ADI) was 4,8 mm, basilar invagination with preserved tectorial membrane was present (fig. 4). There were no signs of bone fracture or compressive myelopathy. Small effusion in atlantoaxial joint was present.
CT scan revealed 50° rotation of the C1 to the left and minor C2 to C3 rotation to the right without luxation or subluxation of facet joints (fig. 5). Basilar invagination of the dens was measured to 6 mm and posterior atlantodental interval (PADI) was measured to 13 mm (fig. 6).
Discussion
AAS is characterized by a loss of stability between the C1 and C2 caused by either traumatic or nontraumatic causes [1]. Nontraumatic AAS combines many different entities, including nasopharyngeal torticollis (Grisel syndrome), atlantoaxial rotator subluxation (AARS), atlantoaxial rotator fixation (AARF), atlantoaxial rotator dislocation, spontaneous hyperemic dislocation and distension luxation [2].
Grisel syndrome usually affects children aged 8-12 years [3] as a result of conditions such as adenotonsilitis, pharyngitis, tonsillar abscess, cervical abscess and otitis media which lead to hyperemia and pathologic relaxation of the transverse ligament of the atlantoaxial joint causing AAS [2]. Its typical presentation with torticollis, cervical pain and signs of infection was evident in our case [3].
Most cases of AAS can be identified on plain radiography but CT scan provides additional information regarding the identification and characterization of AAS [1, 2]. The ADI is measured from the anterior surface of the dens to the posterior surface of the anterior arch of C1 [1]; distance greater than 5 mm in children is indicative of AAS. Another marker is the PADI, measured from the posterior surface of the dens to the anterior surface of the posterior arch of C1 and should normally measure more than 13 mm. The PADI value has 97% sensitivity for predicting neurologic deficit [4]. Diagnostic criteria for basilar invagination is projection of dens for at least 5 mm above the McGregor's line [4]. The ADI and the PADI measures were borderline in our case, however basilar invagination and C1-C2 rotation were observed.
MRI can be used to obtain additional information on cervical spine and soft tissue changes in patients with questionable neurologic status in first 48h after injury and additional information on ligament disruption and its clinical relevance in patients with CT signs of instability [2].
Treatment consists of conservative and surgical options. Conservative methods with cervical collar, halo fixation and halter traction were primarily used in our case [5]. Since they did not provide an accurate position, surgical treatment with craniocervical fusion was required. Surgical treatment is usually indicated in children when one or more of the following is present: neurologic deficit, persistent anterior displacement with ADI more than 4 mm, deformity lasting for more than 3 months, or its recurrence after 6 weeks of immobilization [1].
6 months after the surgery symptoms resolved with only a minor decrease in range of motion (fig. 7).
Teaching points: Nontraumatic AAS should be considered in case of a child with persisting torticollis and signs of infection [1].
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Atlantoaxial subluxation
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures







Imaging Analysis Report
1. Imaging Findings
Based on the provided cervical spine X-ray, CT, and MRI images, misalignment between the atlas (C1) and axis (C2) is observed, suggesting atlantoaxial instability or subluxation (AAS). In certain slices, the following can be noted:
- The atlantodental interval (ADI) between C1 and C2 approaches or slightly exceeds the upper limit of normal for children (5 mm), indicating abnormal joint alignment.
- MRI sequences show local soft tissue swelling and inflammatory changes, as well as enlargement of some lymph nodes, implying adjacent infection or inflammatory response.
- Three-dimensional reconstructed CT images indicate a mild displacement of the odontoid process relative to the atlas, along with signs of basilar invagination (dens surpassing McGregor’s line), suggesting involvement of the cranial base structures.
- No definite fracture lines are visible on imaging; the main findings point to ligamentous laxity and inflammation leading to subluxation.
2. Differential Diagnoses
Based on the child’s symptoms, medical history, and imaging findings, the following should be considered:
- Grisel’s syndrome (non-traumatic atlantoaxial subluxation): Common in children, where upper respiratory tract or ENT infections (such as tonsillitis or pharyngeal inflammation) lead to laxity of the transverse ligament, causing atlantoaxial instability. In this case, the child has neck pain, signs of infection, low-grade fever, and radiographic subluxation consistent with typical presentations.
- Atlantoaxial rotatory subluxation (AARS): Primarily characterized by rotational misalignment of the atlas relative to the axis, often caused by trauma or inflammatory stimuli. Requires CT or dynamic imaging to confirm rotational displacement.
- Other cervical spine infections/inflammatory conditions (such as retropharyngeal abscess): In severe cases, these may lead to cervical spine instability, yet they are usually accompanied by significant soft tissue abscess appearance.
- Rare odontoid anomalies or fractures: Typically associated with a clear history of trauma or congenital developmental abnormalities, none of which are definitively supported in this case.
3. Final Diagnosis
Considering the clinical course (3 months of neck pain and stiffness with sudden worsening), imaging findings (C1-C2 subluxation, mild adjacent soft tissue inflammation), and clinical evidence (low-grade fever, reactive lymph nodes, history of pharyngeal infection), the most likely diagnosis is:
Grisel’s syndrome (non-traumatic atlantoaxial subluxation).
4. Treatment Plan and Rehabilitation Program
Treatment can be divided into conservative management and surgical intervention. The specific approach should be determined by the severity of the child’s symptoms, the degree of subluxation, and the presence or progression of any neurological symptoms.
- Conservative treatment: Includes cervical collar or Halo brace immobilization, along with appropriate anti-infective treatment (if nasal, pharyngeal, or ENT inflammation is present). In cases with mild symptoms and no significant nerve compression, conservative treatment is often the first choice to achieve stable reduction.
- Surgical treatment: If normal alignment cannot be maintained, neurological function is compromised, or conservative management proves ineffective over an extended period (usually ≥6 weeks or 3 months), posterior atlantoaxial fusion or occipitocervical fusion may be considered. The main objectives are to stabilize the atlantoaxial joint and relieve any potential nerve compression.
Rehabilitation and Exercise Prescription (FITT-VP Principle)
Rehabilitation training should be carried out progressively under the premise of ensuring cervical spine stability, tailored to individual needs:
- Frequency: Initially, schedule light neck and shoulder functional exercises 3-4 times a week, combined with low-intensity aerobic activities (e.g., walking).
- Intensity: From low to moderate intensity, avoiding sudden flexion, extension, or rotation of the neck; incorporate isometric neck muscle strengthening.
- Time: Start with 10-15 minutes per session, gradually increasing to 20-30 minutes.
- Type: Focus on gentle range-of-motion exercises and isometric strengthening for the neck, plus lower limb and core strengthening exercises (e.g., simple planks) to support cervical stability.
- Progression: Gradually increase the duration and intensity of training based on cervical stability and pain status. Once symptoms improve and imaging confirms stability, normal activity range may be resumed.
- Volume & Individual Characteristics (Pattern): During the initial phase of bracing or Halo immobilization, the range of motion is limited; exercises should be conducted under the guidance of a professional therapist. If there are other chronic diseases or cardiorespiratory issues, reduce intensity accordingly and monitor closely.
Disclaimer: The above report is provided as a reference-only medical analysis based on current information and does not replace in-person diagnosis or professional medical advice. Specific treatments should be tailored to the patient’s actual condition, and final decisions should be made by a qualified physician.
Human Doctor Final Diagnosis
Atlantoaxial subluxation