Wide spread skeletal bone involvement of brown tumors as initial presentation of primary hyper parathyroidism



Clinical History
A 26-year-old man presented with a history of low back pain for six months and a history of right knee pain and swelling for one month, which had increased in the past week
Imaging Findings
Radiographs of the right knee, pelvis, and lumbar spine demonstrated diffuse osteopenia. A well-defined, multilocular, lytic lesion with a narrow zone of transition and no evident matrix mineralization was seen in the proximal epiphysis and metaphysis of the tibia (Figure 1,2). Multiple well-circumscribed lytic lesions were seen in the pelvic bones, epiphysis of both femoral heads, and left greater trochanter (Figure 3). Mild sclerosis of the endplates in the lumbar vertebrae was noted (Figure 4, 5).
MRI of the knee (Figure 6,13) was performed, which demonstrated a complex multiloculated heterogeneously enhancing solid-cystic lesion with multiple fluid-fluid levels. There was cortical breach posteriorly with extension of the lesion into the adjacent soft tissue. Multiple heterogeneously enhancing T1 hypointense, T2 hyperintense lesions were seen in the distal femur and fibula.
Neck ultrasonography (Figure 14,15) revealed a solid, hypoechoic nodule posterior to the left lobe of the thyroid with a peripheral feeding vessel and rim vascularity. The patient had elevated PTH level-1148.4 pg/ml (normal value-10-55 pg/mL). Fine needle aspiration of the lesion and 99mTc-sestamibi parathyroid scintigraphy was performed, which confirmed parathyroid hyperplasia.
Discussion
Parathyroid adenomas are the most common cause of primary hyperparathyroidism. Brown tumors are focal bony lesions due to bone remodeling from primary or secondary hyperparathyroidism [1].
Symptomatically, patients suffering from hyperparathyroidism usually present with bone pain, renal stones, gastrointestinal and neurological complaints commonly recognized as “bones, stones, groans, and moans. Brown tumors present as slow-growing bone lesions that may cause pain or pathological fractures [1]. When brown tumors are the initial manifestation of hyperparathyroidism, it can simulate a neoplastic process as in our case and cause lot of diagnostic dilemmas. Imaging plays an important role in characterizing these lesions and demonstrating other key diagnostic features of hyperparathyroidism. We should bear in mind that brown tumors should be considered in the differential diagnosis of multiple osteolytic lesions and guide clinicians with appropriate confirmatory investigations to avoid unnecessary and harmful interventions. Proper clinical history and laboratory investigations are important to arrive at the correct diagnosis [3].
Brown tumours are most commonly seen in the mandible, ribs, clavicle, and pelvis. They have variable radiological characteristics. They can be single or multiple, unilocular or multilocular, well-defined/ill-defined, osteolytic lesions, usually with bone expansion, can demonstrate bony destruction and be associated with pathological fractures/soft tissue involvement[3]. The MRI appearance depends on the relative proportion of its components [3]. The lesions may be solid, cystic, or mixed. Solid components are intermediate to low intensity on T1- and T2-weighted images, while the cystic components are hyperintense on T2-weighted images and may have fluid-fluid levels [3]. There can be an enhancement of the solid component and septa.
Parathyroid adenomas are seen as an oval-shaped homogeneously hypoechoic lesion to the overlying thyroid gland [2]. Doppler imaging commonly shows a characteristic extrathyroidal feeding vessel that enters the parathyroid gland at one of the poles. Internal vascularity is also commonly seen in a peripheral distribution in a characteristic arc or rim of vascularity [2]. Color Doppler sonography of the overlying thyroid gland may show an area of asymmetric hypervascularity that may help to locate an underlying adenoma.99mTc-sestamibi scintigraphy and 4D CT’s can help confirm the presence and location of a parathyroid adenoma [2].
Pre-operative 99mTc sestamibi scan helps in accurately localizing the tumour and plays a greater role in localizing ectopic glands, which can help the surgeon in planning the surgical approach[2]. Treatment of hyperparathyroidism is the first step in the management of brown tumours [1]. After appropriate medical management or surgical resection of the parathyroid adenoma, brown tumours may regress, and almost all radiographic changes tend to return to normal. Our patient underwent resection of the parathyroid adenoma, and brown tumours had decreased in size on repeat imaging is done six months post-surgery.
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Parathyroid adenoma causing brown tumors and primary hyperparathyroidism.
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
X-ray knee AP view

X-ray lateral view

X-ray pelvis AP view

X-ray lumbar spine AP view

X-ray umbar spine lateral view

T2 coronal fat-saturated

T2 sagittal

PD FS axial

T1 sagittal

T1 fat sat post contrast

T1 fat sat post contrast

T1 fat sat post contrast

T1 fat sat post contrast

USG neck
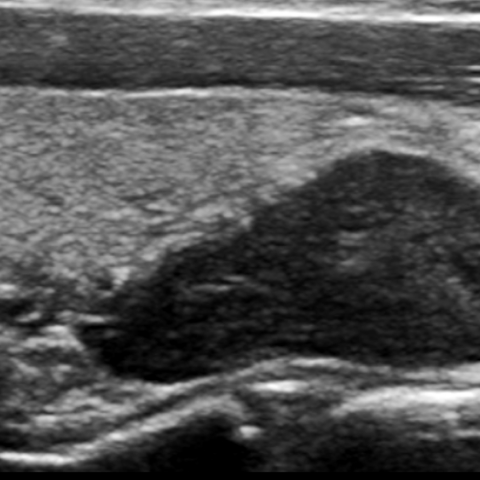
USG neck

1. Radiological Findings
Based on the patient’s X-ray and MRI images, the following features are observed:
- Multiple destructive lesions in the pelvis and lumbar vertebrae, presenting as multiple, variably sized lucent areas (lytic lesions), with disrupted trabecular structure. Some lesions show an expansile change.
- A clearly visible lucent area in the distal femur near the right knee joint, partially well-defined, with thinning of the cortex and slight cortical breakthrough, accompanied by local swelling.
- On MRI sequences, the lesions exhibit heterogeneous signals, including low-to-intermediate signal intensity on T1/T2 sequences as well as cystic or fluid-fluid levels with high T2 signal, suggesting fibrous tissue, hemorrhage, cystic changes, and granulation tissue components within the lesion.
- Color Doppler ultrasound of the neck shows a hypoechoic nodule in the lower anterior region that differs from the thyroid echo. Within it, an oval-shaped high-flow signal is observed, raising suspicion of a parathyroid adenoma.
2. Possible Diagnoses
Based on the radiological findings (multiple osteolytic lesions with expansile changes) and integrating the patient’s lower back and knee joint pain and swelling, as well as suspected hyperparathyroidism, possible diagnoses include:
- Brown Tumor: Resulting from bone remodeling and destruction caused by hyperparathyroidism. It can appear as multiple osteolytic lesions and can be misdiagnosed as metastatic or primary bone tumors.
- Multiple Bone Metastases: Clinically, multiple destructive bone lesions should also raise suspicion of metastatic disease. However, given the relatively young patient and evidence of a parathyroid adenoma, this is less likely.
- Multiple Myeloma: Also presents as lytic bone lesions; however, serum and urine protein electrophoresis usually help clarify the diagnosis. Patients often show anemia, renal dysfunction, etc.
3. Final Diagnosis
Considering the patient’s age, clinical symptoms (low back pain, knee joint swelling), laboratory findings suggestive of hyperparathyroidism (abnormal serum calcium and parathyroid hormone levels), the multiple osteolytic changes on imaging, and the neck ultrasound findings of a parathyroid adenoma, the most likely diagnosis is:
Bone changes (Brown Tumor) due to primary hyperparathyroidism.
4. Treatment Plan and Rehabilitation
Treatment Strategy
- Surgical Treatment: In cases of primary hyperparathyroidism confirmed to have a parathyroid adenoma, surgical excision of the adenoma is the first choice. After surgery, multiple bone lesions may gradually regress or show bone repair over several months.
- Medical Therapy: If hypercalcemia or related symptoms are present, medical intervention such as intravenous fluids, bisphosphonates, etc., may be administered first to lower serum calcium and relieve symptoms.
- Nutritional Support: Pay attention to electrolyte balance and appropriately supplement vitamin D, protein, and so forth to correct metabolic abnormalities and promote bone healing.
Rehabilitation and Exercise Prescription
- Early Stage (1–2 weeks post-op):
- Focus on protective exercises, avoiding wide-range or high-load lower limb activities.
- Under the guidance of medical staff, perform mild muscle contraction exercises daily, for example, isometric contractions of the quadriceps to maintain muscle strength.
- Intermediate Stage (1–2 months post-op):
- After ensuring stable bone lesions, gradually increase weight-bearing exercises. Use resistance bands or light dumbbells for simple lower limb resistance training.
- Incorporate low-impact aerobic exercises, such as a seated or semi-recumbent bike, for 15–20 minutes each session, 3–4 times per week.
- Late Stage (3 months and beyond):
- If follow-up imaging shows bone healing or lesion regression, gradually return to moderate-intensity exercise, such as brisk walking or using an elliptical trainer, 20–30 minutes per session, 3–5 times per week.
- Continue to strengthen resistance training, avoiding heavy-impact loads. Progress gradually and monitor joint and bone response.
The entire rehabilitation process should adhere to the FITT-VP principle (frequency, intensity, time, type, progression, and individualization), with professional clinicians or rehabilitation therapists making timely adjustments based on bone quality, pain levels, and postoperative recovery.
5. Disclaimer
This report provides a reference analysis based on available radiological data and does not replace face-to-face clinical diagnosis and treatment planning. Patients should combine these findings with their own condition and follow the advice of professional doctors and rehabilitation therapists for further evaluation and treatment.
Human Doctor Final Diagnosis
Parathyroid adenoma causing brown tumors and primary hyperparathyroidism.