Rhabdomyolysis after auto-intoxication with antipsychotic drugs


Clinical History
A 20-year old male patient was brought to the emergency department after found lying unconscious (>24h) on his bed due to a suicide attempt with auto-intoxication (antipsychotic and anticholinergic agents). He presented with an expanding skin redness at the right leg/hip region. Blood tests showed elevated serum creatine kinase (20.000 U/L).
Imaging Findings
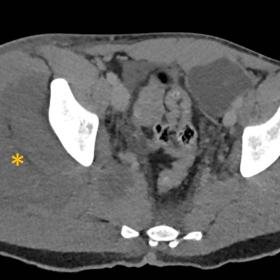
A computed tomography (CT) scan was performed in an emergency setting which showed marked thickening of the proximal quadriceps musculature and gluteal muscles on the right with hypodense areas within (fig 1). On ultrasound, these findings presented as large intramuscular hyperechoic areas (fig 2). MRI demonstrated extended oedema in the affected muscles on STIR imaging (fig 3). Axial T1 pre- and post-contrast images showed a T1- a hypo-intense area with rim enhancement in the gluteal musculature on the right (fig 4). Subcutaneous oedematous changes with limited intermuscular fluid collections were present at the different imaging modalities.
The diagnosis of rhabdomyolysis with myonecrosis and cellulitis was made, based on the combination of symptoms, history, laboratory and imaging findings.
Discussion
Rhabdomyolysis is a potentially life-threatening clinical and biochemical condition caused by direct or indirect muscle damage and is often multifactorial. It results from muscle fibres death and subsequent release of their (potentially toxic) substances into the bloodstream. [1,2] Patient's history and medication use are essential to identify the right cause. Rhabdomyolysis is a possible but infrequent adverse effect of antipsychotic drugs. [3,4]
Typical clinical manifestations are myalgias, myoglobinuria manifested as red-to-brown urine and elevated serum muscle enzymes. [5] Elevated serum creatine kinase of 5× standard value (175 IU/L) is 100% sensitive for the diagnosis of rhabdomyolysis. [2]
Rhabdomyolysis has always been a clinical diagnosis using laboratory findings, physical examination and historical context. Imaging plays a secondary role in diagnosis. It is mainly used to estimate the extensiveness of the affected muscles. Above all, MRI-imaging helps differentiate from other clinically similar pathologies such as necrotizing fasciitis, polymyositis and abscess/pyomyositis which is critical because of the radically different treatment, morbidity and mortality.
Radiography has a limited role (exclusion of associated findings: fractures, joint dislocations) in the diagnosis of rhabdomyolysis; it may show skeletal muscle calcifications four weeks after injury. [5] On ultrasound it can present as muscle swelling, hyperechoic areas of muscle (due to hypercontractility of muscle fibres in the acute phase), hypoechoic areas of muscle (caused by oedema and inflammation of the muscle), architectural distortion (necrosis of the muscle) and fluid within the surrounding muscles. [6,7] On CT, we may visualize hypodense areas with asymmetric muscle swelling and formation of calcifications in later stadia (3-4 weeks) [8,9]. Mild fibre-like enhancement has been described in contrast-enhanced CT, but this must be avoided because of the high risk of renal failure in these patients [5]. MRI is the modality of choice for evaluating rhabdomyolysis. Two types of MRI findings have been described. The presence of rim enhancement is typically for irreversible central myonecrosis (type 2). On both T1-weighted and T2-weighted sequences, there can be a homogeneous signal (type 1: ischemic reaction; overexertion) or heterogeneous (isointense to hyperintense) signal (type 2). [2,5,9].
Our patient's rhabdomyolysis is probably caused by the auto-intoxication of antipsychotics combined with trauma because of prolonged immobilization with long-lasting muscle compression (>24hours). We described a clinical case with several characteristics: (a) severe psychiatric disorder (b) massive overdose with antipsychotics (olanzapine and aripiprazole) and anticholinergic agent (Kemadrin) (c) severe rhabdomyolysis with a positive outcome. The treatment consisted of IV fluid with forced diuresis and antibiotics, and all antipsychotics were withheld during hospitalization.
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Rhabdomyolysis
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
CT

Ultrasound

MRI

MRI

1. Imaging Findings
Based on the provided CT, ultrasound, and MRI images, the following radiological changes can be observed in the right hip and proximal thigh muscle region:
- CT Scan: There is a localized decrease in density within the muscle groups of the right hip and buttock area, primarily at the site labeled with an asterisk in the images, suggesting muscle edema or necrotic lesions. Mild muscle swelling is noted, along with heterogeneous low-density areas in that region.
- Ultrasound: Abnormal echoes are visible within the proximal thigh muscles on the right side, characterized by disordered muscle fiber alignment and local high or low echogenicity with possible small fluid collections, indicating exudation, inflammation, and partial destruction of muscle fibers.
- MRI: Reduced signal in affected muscles on T1-weighted sequences, and markedly high signal on T2 or fat-suppressed sequences, suggesting significant edema and inflammatory changes. Some areas show marginal enhancement, which may correspond to irreversible necrosis or muscle fiber damage.
Overall, these imaging findings are consistent with acute muscle injury and necrosis, localized to the right hip and adjacent thigh muscles, with no significant signs of deep abscess formation or obvious bony lesions.
2. Potential Diagnoses
Based on the imaging characteristics and the clinical history of prolonged immobilization (over 24 hours) after a suicide attempt, the main diagnostic considerations include:
- Rhabdomyolysis
• Commonly occurs after prolonged compression, drug overdose, or ischemic muscle injury. It aligns with the markedly elevated CK (creatine kinase) levels and the corresponding clinical presentation. - Necrotizing Fasciitis
• Typically presents with extensive infection and necrosis involving the skin and deep fascia, often accompanied by severe pain and systemic toxicity. Imaging commonly reveals pronounced fascial thickening, subcutaneous gas, or air-fluid levels. These classic findings are not apparent in the current case. - Other Myositides (e.g., Purulent Myositis, Bacterial or Fungal Infections)
• Imaging may demonstrate abscess-like lesions, and patients often present with fever and significantly elevated white blood cell counts. Although there is a risk of local infection in this patient, the imaging findings point more toward ischemic/necrotic changes rather than a primary infectious etiology.
3. Final Diagnosis
Taking into account the patient’s clinical history (overdose of antipsychotic medication and possible prolonged compression and cold exposure), laboratory results (markedly elevated creatine kinase), and the radiological evidence of widespread muscle edema and necrosis, the most likely diagnosis is:
Rhabdomyolysis
If further clarification of the extent and distribution of muscle necrosis is needed, follow-up ultrasound and MRI studies may be performed, alongside the monitoring of serum enzymes and renal function to assess therapeutic response.
4. Treatment Plan and Rehabilitation
The comprehensive treatment and rehabilitation plan for this case includes the following:
4.1 Treatment Strategies
- Aggressive Fluid Resuscitation and Diuresis: Administer large volumes of intravenous fluids (e.g., normal saline) to prevent acute renal failure, and consider using diuretics (such as furosemide) to facilitate excretion.
- Discontinue Possible Offending Medications: Stop all drugs potentially exacerbating muscle damage or triggering rhabdomyolysis (e.g., high doses of antipsychotics). If continued psychiatric treatment is necessary, ensure careful dose adjustments under close supervision.
- Prevent and Treat Infections: Use antibiotics proactively based on clinical presentation and risk of skin/soft tissue damage to prevent secondary infection.
- Monitor and Support Renal Function: Closely track urine output and renal function indicators (e.g., creatinine, BUN). If there is evidence of significant renal impairment or metabolic acidosis, consider hemodialysis.
- Correct Electrolyte Imbalances: Rhabdomyolysis can lead to hyperkalemia, hyperphosphatemia, and hypocalcemia, requiring timely correction.
4.2 Rehabilitation and Exercise Prescription
Once the patient’s vital signs are stable and the acute phase is under control, gradual rehabilitation training is recommended to promote muscle recovery and overall fitness. Adherence to the
- Frequency: Begin with light activity 1–2 times per day. As muscle strength improves and provided there is no significant pain, progress to 2–3 sessions of simple stretching and low-intensity exercises per day.
- Intensity: Focus on low-intensity exercises initially (e.g., passive joint movements, seated exercises) to avoid re-injury. Increase intensity gradually as the condition improves, introducing mild resistance exercises.
- Time: Start with 5–10 minutes per session, monitoring tolerance. If recovery is favorable, incrementally extend sessions to 20–30 minutes.
- Type: Incorporate assisted manual therapy, range-of-motion exercises, and simple resistance training (e.g., resistance bands, light weights), while avoiding high-impact activities.
- Progression: Closely monitor muscle pain, fatigue, and CK levels. If no adverse reactions occur, modestly increase training volume. Avoid premature or excessive loading to prevent secondary injury.
During recovery, attention should be paid to the following:
- Closely monitor pain or swelling in the affected limb to watch for complications such as compartment syndrome.
- Provide adequate nutritional support, ensuring sufficient protein intake and electrolyte balance for tissue repair.
- For patients with comorbid psychiatric conditions, coordinate care with both psychiatry and rehabilitation services, with emphasis on psychological support.
5. Disclaimer
This analysis report is based on the provided imaging data and clinical background information. It is for medical reference only and should not replace in-person consultation or professional medical advice. Specific diagnostic and treatment decisions should be made by the attending physician, integrating the patient’s individual situation.
Human Doctor Final Diagnosis
Rhabdomyolysis