Radiological aspects of Denosumab-treated giant cell tumour of bone



Clinical History
A 35-year-old male is admitted to our institution’s emergency ward with intense pain and tumefaction in the right wrist. The tumefaction growth had begun insidiously but quick progression in the last weeks and worsening of the pain motivated the patient to seek medical attention. No trauma history was reported.
Imaging Findings
Radiographs of the forearm and wrist were performed and revealed a 10cm lytic expansile lesion in the metaphyseal/epiphyseal region of the right radius, displacing and eroding the lateral cortical surface of the ulna. The margins are ill-defined and the zone of transition is relatively narrow. Despite the aggressive-looking appearance, there is no apparent osteoid matrix or periosteal reaction (Fig. 1).
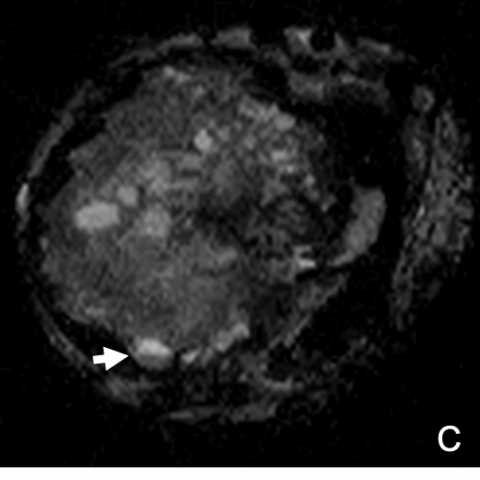
MRI was performed to better characterize the tumour and its relations to adjacent structures. The tumour is predominantly solid, with intermediate signal on T1SE (Fig. 2A) and T2SE and internal cystic areas (Fig.2B), some with fluid-fluid levels (Fig.2C).
As the lesion was deemed to be of difficult surgical management, the patient was subjected to treatment with Denosumab prior to surgery. Follow-up radiographs (Fig.3-4A) and CT (Fig.4B) revealed marked mineralization of the lesion that now possesses a clear and sharp sclerotic margin. No significant reduction of the lesion size was apparent.
Discussion
The lesion was submitted to core biopsy and the already suspected diagnosis of giant cell tumour (GCT) of bone was confirmed. Histological confirmation is required to establish the diagnosis[1]. GCTs are typically found after the closure of growth plates and peak incidence occurs in the 3rd decade[2]. GCTs of bone are usually benign tumours, but local recurrences are common (up to 60%)[3].
Metastatic involvement (especially to the lungs) and sarcomatous transformation have been reported, but are rare. Histologically, the tumour is characterized by the presence of giant cells in a background of mononuclear stromal cells, with increased osteoclastic activity due to activation of nuclear factor-kappa B ligand (RANKL)[2,4].
These lesions tend to be eccentrically located in metaphyseal/epiphyseal regions, near articular surfaces. The most common radiographic appearance is that of a lytic lesion with well-defined non-sclerotic margins. Some might present with a more aggressive appearance, with cortical thinning, expansible remodelling or cortical bone destruction, as was our case. Typical signal characteristics in MR include low-signal in T1-weighted images, high-signal in T2-weighted images and enhancement of solid components after paramagnetic contrast administration. A low-signal-intensity margin, representing osseous sclerosis or a pseudocapsule, is a common finding. Fluid-fluid levels may be observed, in association with aneurismal bone cyst (ABC) components. These components are common in GCTs (14% of lesions) and, when prominent, contribute to a more aggressive radiographic appearance[5].
For larger and more destructive GCTs wide resection and reconstruction with allografts and/or metal prostheses may be necessary. However, in large lesions, complete resection may be difficult and joint reconstruction can be challenging, with great morbidity. Recent studies support that most patients show objective tumour response to Denosumab which should be assessed by the response criteria by inverse Choi density/size (ICDS)[5-7]. The dynamic response to Denosumab is characterized by a change in lesion density rather than size reduction, inducing internal mineralization, marginal sclerosis and better demarcation of lesions. The changes should be monitored with a combination of radiograph and CT, as the latter allows the use of Hounsfield Units (HU) as an objective measure of response[6-8].
Results from previous studies concluded Denosumab decreased the local staging of GCT, allowing curative surgical resection in approximately 57% of patients. However, it does not prevent recurrence in patients with prior surgical treatment and should not be used as adjuvant therapy[8].
The patient refuses surgery, currently maintaining Denosumab therapy.
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Giant cell tumour of distal radius treated with Denosumab
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures







Medical Analysis Report
I. Imaging Findings
The patient in this case is a 35-year-old male, primarily presenting with progressive swelling and pain in the right wrist. X-ray and MRI examinations show:
- Local expansile osteolytic lesion in the distal radius with disordered trabecular structure, relatively well-defined borders but no obvious sclerotic rim.
- Thinned cortex with areas of expansion or a "blown-out" appearance, indicating significant cortical destruction and remodeling by the lesion.
- On MRI, the lesion appears hypointense on T1-weighted images (T1WI) and hyperintense on T2-weighted images (T2WI), with fluid-fluid levels in some regions suggesting aneurysmal bone cyst (ABC)-like components within the lesion.
- After contrast enhancement, the solid component shows enhancement and the lesion margins become clearer. A peripheral low signal band may be observed, potentially reflecting a sclerotic border or pseudocapsule.
- No obvious extensive soft tissue involvement is noted, though there is local soft tissue compression or mild infiltration. Structures near the wrist joint are affected, impacting adjacent joint structures.
II. Potential Diagnoses
Based on the patient's age, the lesion's location in the epiphysis-metaphysis region (especially near the articular surface), and the imaging features, the following diagnoses are considered:
- Giant Cell Tumor of Bone (GCT)
Reason: Commonly occurs around the metaphyseal-epiphyseal region of long bones near the closed growth plate; often presents as expansile osteolysis and may be associated with aneurysmal bone cyst-like changes; frequently seen in patients aged 20–40; pathology in this case has confirmed GCT. - Aneurysmal Bone Cyst (ABC)
Reason: Fluid-fluid levels on imaging and an expansile appearance are often noted; however, this usually appears in adolescents, and in this case, the patient’s age is older and the lesion more closely matches GCT features, making ABC less likely. - Rare Possibility of Osteosarcoma or Chondrosarcoma
Reason: If the lesion were extremely aggressive with widespread bone destruction and a large soft tissue mass, a malignant tumor would need to be excluded. However, this case lacks typical sarcoma characteristics and histopathology confirms GCT, making a malignant transformation less likely.
III. Final Diagnosis
Considering the patient's age, clinical presentation, imaging findings, and pathological biopsy results, the most likely diagnosis is Giant Cell Tumor of Bone (GCT).
According to the data, a biopsy has been performed and histologically confirmed. The patient is currently receiving Denosumab treatment, further supporting the diagnosis and treatment strategy for GCT.
IV. Treatment Plan and Rehabilitation
1. Treatment Strategy Overview
- Surgical Treatment: For giant cell tumors of bone, if the lesion is relatively localized, thorough curettage and bone grafting (or joint reconstruction) is a common curative approach. However, the patient in this case currently refuses surgery.
- Medical Therapy: Denosumab can inhibit osteoclast activity, reducing tumor expansion. It may also help shrink the lesion or diminish surgical difficulty in some cases. Reports suggest that Denosumab can achieve objective responses in GCT treatment.
- Radiotherapy: This can be considered in patients who are not surgical candidates or those with high surgical risks, though it is not the first choice for benign lesions.
- Follow-Up: Periodic imaging follow-up (using X-ray, CT, or MRI) is required to monitor lesion stability and changes in bone quality.
2. Rehabilitation and Exercise Prescription
In this case, the primary issues are severe bone destruction in the right wrist and pain. While protecting the lesion area, maintaining joint function and strengthening upper limb muscles is necessary. Rehabilitation and exercise prescriptions should follow the principles of gradual progression, individualization, and safety. A possible plan is outlined below:
- Early Stage (Protection Phase):
- Use a wrist brace or external fixation device to protect the affected wrist, reducing excessive loading and unnecessary twisting.
- Perform active movements of the shoulder and elbow joints to avoid joint stiffness or muscle atrophy.
- Practice simple wrist flexion-extension exercises within a pain-free range, performed 2–3 times a day for about 5–10 minutes each time.
- Intermediate Stage (Functional Training):
- As the lesion stabilizes or symptoms improve, gradually increase the active range of motion exercises for the wrist, along with forearm pronation and supination.
- Engage in low-intensity exercises using a resistance band or grip strengthener with slow, controlled movements, avoiding excessive load. Each session lasts 10–15 minutes, 3–4 times per week, with gradual increases based on tolerance.
- Late Stage (Load-Bearing Reinforcement):
- If bone density improves and structural stability is achieved, gradually introduce strength training (e.g., light dumbbells or wrist weight exercises) under the guidance of a physician or therapist.
- Throughout the rehabilitation process, continually monitor wrist stability and pain levels, and communicate with the therapist after each exercise session.
FITT-VP Principle (Frequency, Intensity, Time, Type, and Progression):
Start at a lower frequency (2–3 times per week), with intensity at a level where the patient experiences mild to moderate fatigue, working 10–15 minutes per session and gradually extending the duration. The focus is on joint mobility and muscle strengthening, evaluated every 1–2 weeks. Progress is based on stability and pain level.
Disclaimer: This report is a reference-oriented medical analysis and cannot replace in-person medical consultation or professional advice. Specific treatment and rehabilitation recommendations must be determined by a clinical physician and rehabilitation therapist based on the individual patient’s condition.
Human Doctor Final Diagnosis
Giant cell tumour of distal radius treated with Denosumab