An unusual case masquerading as lateral patellar instability



Clinical History
A 27-year-old female patient presented with a 12-month history of recurrent anterior knee pain, instability and a ‘clicking’ sensation aggravated by activity, with no preceding traumatic injury. The patient had tenderness overlying the lateral border of the patella and the remainder of the clinical examination was normal, including a negative patellar apprehension test and absent ‘J’ sign.
Imaging Findings
Presentation MRI:
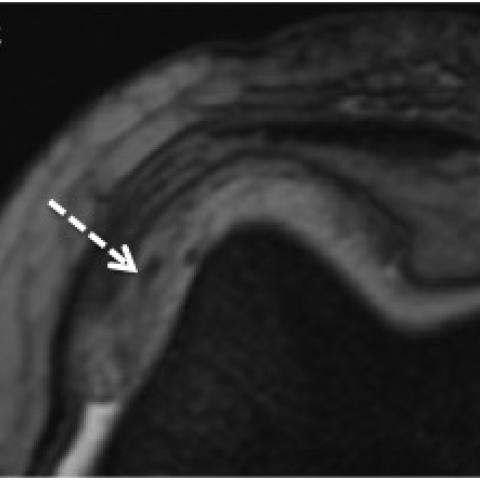
- Increased signal within the superolateral aspect of Hoffa’s fat pad on PD FS and T2 sequences, attributed to oedema secondary to patellar mal-tracking (Figure 1).
- No contusions to the medial patella or lateral femoral condyle to suggest recent lateral patellar dislocation.
- Normal medial patellofemoral ligament.
- No features of trochlear dysplasia or patella alta.
- Normal tibial tuberosity – trochlear groove distance of 10 mm.
There was no clinical improvement after 8 months of conservative management with physiotherapy and repeat MRI was performed to re-assess for a surgical target:
- Marked progression of the lesion within Hoffa’s fat pad, which had increased in size and was now more mass-like, with low signal intensity foci on PD FS and T2 sequences (Figure 2A and 2B).
- Gradient echo imaging was performed, which demonstrated blooming artefact within the lesion in keeping with haemosiderin deposition and localised pigmented villonodular synovitis (PVNS) (Figure 2C).
- The mass was relatively laterally subluxed on the gradient echo sequences when compared with the earlier PD imaging (Figure 2).
Discussion
This case is an example of a rare pathology, PVNS, manifesting with common mechanical symptoms of lateral patellar instability. PVNS is a benign proliferative condition affecting the synovial lining and both diffuse and localised patterns have been described [1]. The aetiology remains unclear, however cytogenetic studies suggest that a neoplastic process is most likely [2]. PVNS can affect any large joint, however the knee is most commonly involved and accounts for 80% of cases [1]. PVNS of the knee usually presents insidiously with generalised pain and recurrent swelling, and symptoms are frequently present for many months prior to diagnosis [1].
Lateral patellar instability most frequently occurs in active females in the second decade of life [3]. Over half of cases of initial patellar dislocation are secondary to a sporting injury and MRI is indicated to assess for predisposing morphological factors, including trochlear dysplasia, patella alta and a raised tibial tuberosity – trochlear groove distance, which can be targeted surgically [4]. PVNS is a very rare cause of lateral patellar instability, with a single case previously reported in which nodular disease within the medial patellofemoral joint resulted in mass effect on the patella and lateral subluxation [5]. To the best of our knowledge, we report the first case of localized patellofemoral PVNS subluxing laterally and masquerading as patellar instability, highlighting to radiologists the importance of considering more unusual pathologies as a cause for common symptoms, especially when no other clear cause is identified.
MRI is the imaging modality of choice for the diagnosis of PVNS, which typically presents as a synovial based mass with hypointense foci on T1 and T2 weighted imaging [1]. Iron within the haemosiderin deposited in PVNS causes local magnetic field inhomogeneity, resulting in the characteristic susceptibility (blooming) artefact on gradient echo sequences [6]. Although a rare condition, imaging features are characteristic and help differentiate PVNS from other synovial based pathologies. Treatment of PVNS consists of total synovectomy, which is curative, however recurrence rates of between 30% and 50% have been reported [2].
Take home message:
- Lateral patellar instability is most commonly mechanical, but rare causes should be considered particularly when no predisposing factors for instability are identified on imaging.
- Blooming artefact on gradient echo sequences helps secure the diagnosis of PVNS and should be considered when there is suspicion on standard MR sequences.
- Interval imaging can be helpful in cases when clinical symptoms of lateral patellar instability progress.
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Localised pigmented villonodular synovitis
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures




Medical Analysis Report
1. Imaging Findings
The patient’s knee MRI images show the following:
1. A focal soft tissue lesion in the synovium near the lateral articular surface of the patella, manifesting as a prominent or nodular change.
2. In T1- and T2-weighted sequences, the lesion exhibits heterogeneous signals with multiple low-signal areas (possibly indicating hemosiderin deposition).
3. On gradient echo (GRE) or similar susceptibility sequences, there is a pronounced “magnetic susceptibility artifact” or “blooming effect,” suggesting a significant amount of iron-containing hemosiderin within the lesion.
4. The lesion is primarily confined to the lateral synovium of the patellofemoral joint, with no obvious erosive bone changes or extensive bone involvement.
2. Potential Diagnoses
- Conventional Lateral Patellar Subluxation (Instability): Often attributed to structural causes such as anatomical abnormalities of the patellofemoral joint (high-riding patella, shallow trochlear groove, tight lateral support structures, etc.). However, in this case, common etiologies are not evident, and MRI indicates abnormal synovial proliferation.
- Pigmented Villonodular Synovitis (PVNS): Commonly seen in the knee. On MRI, it often presents as uneven synovial proliferation accompanied by low-signal foci on T1- and T2-weighted sequences and a blooming effect on GRE sequences. This correlates with the patient’s symptoms (instability, soft tissue “swelling” or “mass effect”) and the lesion location.
- Other Synovial Lesions (e.g., synovial chondromatosis, intra-articular synovial proliferative pathologies): They can show synovial inflammation or nodular proliferations, but the hemosiderin deposition is usually not as characteristic as in PVNS.
3. Final Diagnosis
Considering the patient’s age, symptoms (recurrent anterior knee pain, clicking or discomfort with movement), duration (one year), clinical exam findings (no typical mechanical signs of patellar instability), and the characteristic MRI findings of iron-containing hemosiderin deposition, the most likely diagnosis is:
Pigmented Villonodular Synovitis (PVNS).
4. Treatment Plan and Rehabilitation Program
Treatment Strategy:
- Surgical Treatment: For localized PVNS, arthroscopic or minimally invasive synovectomy (synovial or lesion excision) is the primary treatment option. It helps reduce recurrence risk and restore joint function.
- Adjunct Therapy: In cases of extensive disease or high recurrence risk, radiation therapy may be considered based on patient age, lesion extent, and postoperative recovery.
- Postoperative Follow-Up: PVNS has a certain recurrence rate, thus regular follow-up and imaging are required. If knee pain or instability recurs, repeat MRI should be performed to rule out recurrence.
Rehabilitation and Exercise Prescription:
The rehabilitation program should follow a “gradual and individualized” approach, divided into the following phases:
-
Early Postoperative Period (Weeks 1-2):
- Main goals are to alleviate pain and reduce joint swelling through methods such as cold compress, limb elevation, and gentle movement.
- Passive or assisted active exercises are recommended with limited range of motion, avoiding vigorous weight-bearing activities.
-
Intermediate Postoperative Period (Weeks 2-6):
- Gradually initiate active knee range-of-motion exercises and strengthen quadriceps control (e.g., straight leg raises, small-range knee flexion and extension in seated or partial squat positions).
- Weight-bearing exercises should be introduced gently, potentially using resistance bands or water-based therapy if available, progressively increasing resistance and repetition.
-
Late Postoperative Period (6 Weeks and Beyond):
- Once joint range of motion has largely recovered, incorporate more functional exercises, such as light jogging and stair climbing.
- Continue reinforcing stability and coordination of the knee’s surrounding musculature, combined with core strength exercises.
Following the FITT-VP principle (Frequency, Intensity, Time, Type, Progression, and Individualization), training sessions can be gradually increased to 3-5 times a week, each lasting 20-40 minutes, with progressive intensity increments. Adjust the regimen based on knee response and pain levels; reduce or pause activities as needed.
5. Disclaimer
This report is based on the provided case information and imaging results. It is for medical reference only and cannot replace an in-person diagnosis or professional evaluation by a qualified physician. If you have any questions or your symptoms worsen, please seek prompt medical attention and follow the advice of a specialist.
Human Doctor Final Diagnosis
Localised pigmented villonodular synovitis