A case of primary Ewing’s sarcoma of skull in a pediatric patient presenting with hydrocephalus



Clinical History
Parents of a 2-year-old female presented to pediatric OPD when they noticed progressive swelling of patient’s head since 1month. They also noticed visual disturbance, difficulty in walking since 20 days, fever and episodes of vomiting in last 2 days. No history of trauma/ seizures/ loss of consciousness.
Imaging Findings
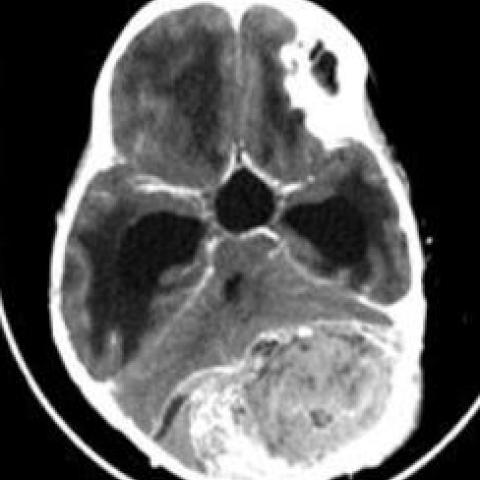
CECT Brain showed fairly well defined lobulated heterogeneous soft tissue density lesion (35-45 HU) measuring 5.1x9.4x.4.9 cm (AP X TR X CC) epicentered in occipital bone on left side showing internal chunky calcification (Figure 1) causing extensive destruction of inner and outer tables with sunburst pattern of periosteal reaction(Lodwick Type III) with intracranial (involving extra-axial space) and extracranial components (Figure 2).
On contrast study, the lesion showed heterogeneous enhancement with few areas of hypodense necrosis.
Anteriorly, there was displacement of left cerebellar hemisphere and mass effect on brain stem with displacement of basal cisterns and ascending transtentorial herniation. It was causing upstream dilatation of third and bilateral lateral ventricles with periventricular CSF seepage - obstructive hydrocephalus.
There was no evidence of infiltration into brain parenchyma (Figure 3).
It was displacing left transverse sinus and straight sinus.
Medially, the lesion was crossing midline and causing displacement of right cerebellar hemisphere.
Bilateral optic nerves appeared tortuous with flattening of posterior globe- papilledema.
Discussion
Ewing sarcoma (ES) is a malignant small, round cell tumour arising from bone and soft tissue in children and young adults. It can occur at osseous and extra osseous sites [1].
There is male predilection in the ratio of 1.8 : 1. Approximately 90% of cases occur in the first two decades of life, peak incidence being between 5 and 13 years [2].
The mesenchymal stem cell is proposed as the cell of origin, but there could be other cell types that may give rise to this tumour based on its ability to occur at multiple sites [3]. Its usual locations are diaphysis of long bones followed by pelvis, ribs, vertebrae, and rarely skull (1).
Intracranial involvement is rare, with a reported incidence of 1-6% of all cases. Calvarial involvement is found in <1% patients [4]. Temporal bone is commonly involved followed by parietal and occipital bone. Sphenoid and ethmoid bones involvement is less seen [2].
Ewing’s sarcoma typically grows extradurally; usually, large mass is seen before dural invasion or clinical detection or both. The duration of symptoms ranges from 2 weeks to 2 years. Symptoms develop as a result of dural invasion or raised intracranial pressure. Headache and scalp swelling are the most common symptoms, papilloedema is the most common sign. However, these rarely present with hydrocephalus [2].
Histologically, characteristic feature include sheets of small round blue cells with an increased nucleus-to-cytoplasm ratio. Pseudorosettes may be present. Mitoses are common. Bony spicules may be present, and CD99 and vimentin may be expressed [2].
The chromosomal translocation t(11;22)(q24;q12) is pathognomonic [5].
The CT scan usually shows an isodense mass that may extend intra- or extracranially. The enhancement is usually strong and heterogeneous. There may be bony destruction and/or new bone formation, with a spiculated pattern distinctive of Ewing’s sarcoma. The MRI imaging shows heterogeneous signal intensity, along with scattered areas of haemorrhage and necrosis [2].
Anaemia, leukocytosis, elevated levels of ESR, ALP and C-reactive protein seen. An elevated LDH level is associated with a poor prognosis [6].
Age <15years, female gender, absence of metastases at diagnosis, no regional lymph node involvement, peripheral location of the tumour, tumour <8 cm, and initial LDH< 170 IU/L favours good outcome [6].
Surgery remains the best treatment modality. Adjuvant therapy after resection including radiotherapy and chemotherapy is essential [2,7].
Cranial Ewing’s sarcoma rarely shows early metastasis and has a better but still severe prognosis compared to many counterparts [8].
Differential Diagnosis List
Final Diagnosis
Ewing’s sarcoma
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures







Medical Analysis Report
I. Radiological Findings
The patient is a 2-year-old female, presenting with progressive cranial swelling, fever over the past two days, and recurrent vomiting. The main CT (plain and contrast) findings are as follows:
- Multiple osteolytic lesions in the skull with irregular destruction and changes in new bone formation.
- Masses visible both extracranially and intracranially, forming irregular nodular lesions with pronounced enhancement in certain areas.
- Extensive lesions involving the cranial vault with inward growth, producing a space-occupying effect; the ventricles appear compressed and deformed, indicating obstructive hydrocephalus.
- Marked local soft tissue swelling; enhanced CT scans show significant, irregular enhancement suggesting a lesion with rich blood supply.
- Destruction of the diploë (cancelous layer) observed in some sections; inner and outer tables appear incomplete, with the lesion extending into the epidural or subcutaneous tissue.
II. Potential Diagnosis
Based on the patient's age, clinical symptoms, and imaging features, the following possible diagnoses or differential diagnoses are considered:
- Ewing’s Sarcoma
- Neuroblastoma Metastasis to the Skull
- Lymphoma or Leukemia Infiltration of the Skull
- Langerhans Cell Histiocytosis (LCH)
Commonly seen in children and adolescents, classified as a small round cell malignant tumor. It often affects long bones or flat bones, including the skull. CT imaging may show osteolytic destruction alongside “onion-skin” type periosteal reaction. Clinically, patients can present with local swelling, pain, and raised intracranial pressure.
Neuroblastoma frequently occurs in young children and may metastasize to the skull or epidural space. However, such metastases typically appear after an evident primary lesion in the abdomen or chest is identified.
In children, skull involvement can occur in lymphoma or leukemia. Generally, other systemic symptoms are also noted, such as generalized lymphadenopathy or abnormal hematologic findings. Imaging often reveals multiple areas of bone destruction.
LCH may involve the skull, often presenting as “punched-out” osteolytic lesions. However, the overall aggressiveness is usually less pronounced than that of Ewing’s sarcoma, and associated scalp lesions or skin/ear discharge may be more common.
III. Final Diagnosis
Considering the patient’s age (2 years), clinical presentation (head swelling, symptoms of raised intracranial pressure, possible visual disturbances, gait instability), and the above-mentioned CT findings and literature review, Ewing’s Sarcoma aligns most closely with the overall presentation. A definitive diagnosis typically relies on pathological examination (small round cells, immunohistochemical staining positive for CD99 and vimentin, or the characteristic chromosomal translocation t(11;22)).
IV. Treatment Plan and Rehabilitation Program
Ewing’s sarcoma generally requires a comprehensive treatment strategy. The following approach is recommended:
1. Surgical Treatment
- For resectable lesions, tumor resection can be performed to reduce intracranial pressure and alleviate neurological symptoms.
- After gross or subtotal resection, close coordination with radiotherapy or chemotherapy is essential.
2. Radiotherapy and Chemotherapy
- Following surgery, or in cases where the tumor is large and cannot be completely removed, radiotherapy may be employed to control the local lesion.
- Chemotherapy often includes multiple agents (e.g., doxorubicin, cyclophosphamide, vincristine) administered in cycles to decelerate progression and reduce recurrence.
- Throughout treatment, regularly monitor complete blood counts, liver and kidney function, and continually evaluate therapeutic efficacy and adverse reactions.
3. Rehabilitation and Exercise Prescription
Rehabilitation should be individually tailored and progressed gradually at each stage of treatment. For this young patient, professional guidance from a rehabilitation therapist or pediatric specialist is advised:
- Early Stage Rehabilitation (during hospitalization or early post-surgery)
- The primary goal is to prevent complications from prolonged bed rest, including gentle passive movements and activities like sitting on the edge of the bed.
- Under parental supervision, perform mild joint mobilizations to maintain muscle and joint flexibility.
- Mid-Stage Rehabilitation (after initial control of the disease)
- If the condition stabilizes without new adverse events, gradually introduce low-intensity active exercises, such as short-distance walking or standing balance training.
- Practice sessions can be done 2-3 times daily for 5-10 minutes each, monitoring the child’s tolerance and adjusting accordingly.
- Late-Stage Rehabilitation (when the condition is stable or in maintenance)
- Incorporate play-based therapy according to the child’s interests, such as light ball-kicking or building block games, to ensure sufficient activity while promoting flexibility and coordination.
- Gradually increase the intensity and duration of activities. If permitted by the condition, aim for about 20-30 minutes of light-to-moderate exercise per day, possibly split into shorter sessions.
Throughout the rehabilitation process, closely observe the child’s temperature, wound healing, and overall tolerance. Adhere to the FITT-VP principle (Frequency, Intensity, Time, Type, Progression, and Individualization) to maximize rehabilitation benefits while maintaining safety.
Disclaimer: The above analysis report is for reference only and cannot substitute for in-person clinical diagnosis or professional medical advice. For any specific treatment plan, please consult a specialist or visit the hospital.
Human Doctor Final Diagnosis
Ewing’s sarcoma