Large-sized pilomatrixoma of the right elbow: MRI case report on a middle-aged patient



Clinical History
This case report focuses on uncommon benign neoplasm on the right elbow of a 39-years-old male patient. The patient underwent MRI examination, as requested by his personal General Practitioner (GP), with pre and post-contrast medium administration at the Department of Radiology of our local hospital.
The execution of MRI was justified to evaluate the likely presence of a connective tissue capsule and its peritumoral standing. In fact, we suspected that such lesion was infiltrating the muscles of the patient’s forearm. This skin lesion was characterized by slow-growth path (diameter 7 cm) and reddish colour as illustrated in Fig.1.
Imaging Findings
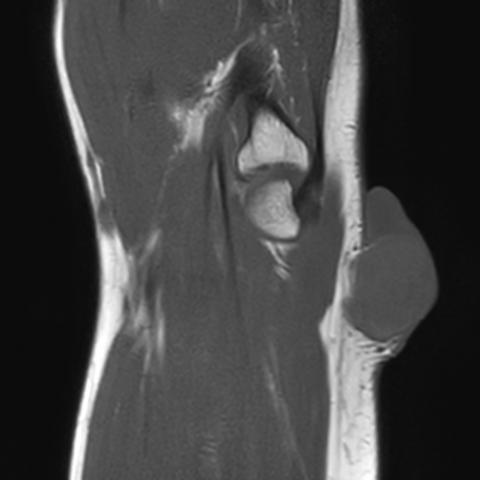
Imaging findings discover a neoplasm of cutaneous and subcutaneous tissue with oval shape and clear margins. We perform a two-stages study via MRI: pre and post-contrast agent administration. First, MRI highlights the main features as isointense signal to skeletal muscle on T1-weighted image (Fig.2) and heterogeneous signal in T2-weighted image with area of high Signal Intensity (SI) mixed with area of low SI (Fig.3).
Area with low SI is compatible with fibrosis as well as calcifications. Although, the patient executes neither Radiography nor Computed Tomography (CT), the presence of calcifications is documented by histological report, after surgical intervention.
No altered signal intensity on diffusion-weighted imaging (DWI) is found (Fig. 4.A and 4.B). Then, after the administration of contrast agent, MRI detects the presence of heterogeneous enhancement on central and peripheral parts (Fig. 5.A). Besides, the enhancement is marked in the sequence with Fat-Suppression, obtained immediately after the first T1-weighted post-contrast sequence (Fig. 5B).
The existence of several calcifications provides differential diagnosis of Pilomatrixoma both with benign lesions, such as the osteoma cutis, and malign neoplasms, such as the soft-tissue osteosarcoma. Although the osteoma cutis is too small for being studied by MRI, osteosarcoma of soft tissues exhibits similarities with Pilomatrixoma. In fact, all aforesaid lesions have well-circumscribed heterogeneous mass lesion that are isointense to muscles on T1 and have high SI on T2-weighetd images. On the other hand, the main difference between Pilomatrixoma and osteosarcoma consists that the latter neoplasm presents haemorrhage or necrotic areas, which appears as high signal foci on both T1 and T2 (due to methemoglobin) or low signal foci on 2 (due to hemosiderin) [1].
Then, Pilomatrixoma has similarities with fibrosarcoma in extremities because they share same heterogeneous SI on T2-weighted image and enhancement after contrast medium administration. However, fibrosarcoma has the band-like areas of low signal on both T1WI and T2WI, oedema signals in the peritumoral muscle and, in some cases, also on the involved adjacent bone, such as Pilomatrixoma [2].
Furthermore, Pilomatrixoma presents differential diagnosis with other skin neoplasms. First, we compare Pilomatrixoma with the squamous cell carcinoma that exhibits intermediate to low signal on T1, intermediate to high signal on T2 and enhancement on T1 C+ (Gd) with fat saturation. However, the squamous cell carcinoma is characterized by hyperkeratotic nodules that can develop ulceration and ill-demarcated deep tumour margins (60%) and peritumoral fat stranding (93%) [3].
Besides, the long-standing foreign body granuloma, that has a capsule with low signal on T1 and T2, differs from Pilomatrixoma due to the linear peripheral enhancement of the former showed via MRI.
Finally, we also study the dermoid cyst due to its fluidlike signal with variable low-signal component on T2, multiple layers of keratin debris and intraluminal calcifications [4]. Besides, the dermoid cyst has high signal on DWI, central nonenhancement and peripheral thin rim enhancement after the usage of gadolinium MRI contrast agent. Thus, dermoid cyst differs from Pilomatrixoma because this latter shows-off heterogeneous enhancement and lack of restricted diffusion. [5]
Discussion
Pilomatrixoma is first described by Malherbe and Chenantais in 1880, as a superficial benign soft-tissue tumour [6]. Aggressive growth path of the tumour has been encountered rarely. Usually, the common site where this lesion arises, as a solitary nodule, is located on head and neck region (64%) [7, 8]. Frequently, it occurs in patients younger than 20 years old and the peak of incidence is registered between 8 and 13 years old, with mild female preponderance (female-to-male ratio 1.15:1) [8].
During a clinical examination, Pilomatrixoma measures less than 3 cm in diameter and such characteristics lead dermatologists to misrecognize it as epidermoid cysts [9].
Current scientific literature shows that Pilomatrixoma could be associated with Gardner’s syndrome, myotonic dystrophy, Turner’s syndrome, trisomy 9 and Sotos syndrome [8, 5]. Furthermore, as reported by Bulman et al., in a research conducted by Gat et al. (1998), several cases of pilomatrixoma show-off a mutation in the beta-catenin gene (CTNNB1) which is responsible to influence the terminal differentiation of the hair follicle cells during embryogenesis. In addition, they report that the diagnosis of Pilomatrixoma, made on children with superficial soft-tissue lesions, is frequently mistaken among pediatric radiologists because of their lack of awareness of its likely occurrence [5].
On Ultrasound (US), the main features of Pilomatrixoma, described in literature, are hypoechoic rim and internal reticulations, posterior shadowing and the location of the tumour at the junction of the dermis and the subcutaneous fat [5, 10]. On CT, the main characteristics of Pilomatrixoma are calcifications and a mild to moderate enhancement after contrast medium administration [8,5,11]. The surgical excision is the only curative treatment [12] (Fig. 6). In addition, this case report gives an outstanding contribute to the existent literature by indicating helpful guidelines to study this pathology with the aid of MRI. In fact, the role of MRI is to help clinicians to assess the locoregional staging of cutaneous diseases. Besides, the usage of MRI is helpful because it permits to show the existence of a connective tissue capsule and to exclude the presence of peritumoral stranding.
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Pilomatrixoma
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures





Medical Imaging Analysis Report
1. Imaging Findings
Based on the provided right elbow (MRI) images and clinical information, the following observations can be noted:
- A relatively well-defined round or ovoid soft tissue mass is visible subcutaneously around the elbow joint. It measures approximately 7 cm, presents a marked protrusion, and is visibly reddish on the surface.
- On MRI, the lesion shows slightly isointense or mildly hypointense signal on T1WI and slightly hyperintense signal on T2WI, with clear demarcation from the surrounding soft tissue. On contrast enhancement, mild to moderate enhancement is observed in some areas.
- The lesion is located at the interface between the skin and subcutaneous fat. A distinct capsule or encapsulation feature is noted, without obvious invasion into adjacent muscles or tendons.
- No significant bone destruction or periosteal reaction is observed.
2. Potential Diagnoses
Based on the imaging features and the patient's clinical characteristics, possible diagnoses or differential diagnoses include:
- Epidermoid Cyst: Often forms subcutaneously, typically less than 3 cm in diameter. Although it grows slowly and can adhere to the skin surface, it may be confused with the lesion in question.
- Lipoma: A common benign tumor of adipose tissue, usually well-circumscribed. On MRI, lipomas characteristically show fat signal on T1WI and T2WI. However, this lesion is less likely to be a lipoma due to the atypical enhancement and tissue characteristics.
- Giant Cell Tumor of Tendon Sheath: Commonly found around tendons, can present as a localized mass, but its typical MRI enhancement pattern and predilection for the fingers or wrist region do not completely match the location and appearance of this lesion.
- Pilomatrixoma: A benign tumor derived from hair follicle matrix cells that may feature calcification. Typically adherent to the skin and often occurs in the head, neck, and upper extremities. In this case, the MRI shows a capsule and local enhancement after contrast, along with a clinically noticeable skin protrusion, which is highly suggestive of pilomatrixoma.
3. Final Diagnosis
Taking into account the patient’s age, the characteristics of the mass (slow growth, up to 7 cm in diameter, reddish surface), MRI findings (encapsulated, confined to the subcutaneous layer, no obvious muscle or bone involvement), and considering the postoperative pathology findings, the most likely diagnosis is:
Pilomatrixoma
If a pathological diagnosis has not yet been obtained, surgical excision and pathological examination are recommended for confirmation.
4. Treatment Plan and Rehabilitation Program
4.1 Treatment Strategy
- Surgical Excision: For a large pilomatrixoma in the elbow region, complete surgical excision is the most common and effective treatment. If the pathology confirms a capsule and no adhesion to surrounding tendon structures, efforts should be made to preserve functional integrity during surgery.
- Medication: Generally, no specific drug therapy is needed for this tumor. If necessary, antibiotics may be used to prevent postoperative infection and analgesics for symptomatic pain relief.
- Follow-Up: Regular outpatient visits are recommended to monitor the wound healing process, check for any signs of recurrence, and manage complications if they arise.
4.2 Rehabilitation/Exercise Prescription
Postoperative rehabilitation focuses on restoring range of motion in the elbow joint and improving the function of surrounding soft tissues. A stepwise plan following the FITT-VP principle can be considered:
- Early Postoperative Phase (Wound Healing Period)
- Frequency: 1–2 times per day
- Intensity: Low intensity, primarily passive movements and gentle active movements
- Time: 5–10 minutes per session to prevent joint stiffness
- Type: Gentle flexion and extension of the elbow joint (within a pain-free range), combined with cold compress or physical therapy to reduce swelling
- Progression: Gradually increase the range of motion based on wound healing and pain tolerance
- Intermediate Recovery Phase (Wound Healed, Increased Range of Motion)
- Frequency: 3–4 times per week
- Intensity: Low to moderate, may include light resistance training with elastic bands
- Time: 15–20 minutes per session, with intermittent rest
- Type: Under the guidance of a rehabilitation therapist, perform active range-of-motion exercises and light muscle strengthening (biceps, triceps), along with overall gentle exercise
- Progression: Increase resistance and duration progressively in the absence of significant swelling or pain
- Late Postoperative Phase (Functional Reinforcement)
- Frequency: 3–5 times per week
- Intensity: Moderate, can be raised based on individual tolerance
- Time: 20–30 minutes per session
- Type: Combine upper limb functional training with whole-body aerobic exercises (e.g., brisk walking, swimming). Include stability and proprioceptive training for the elbow joint.
- Progression: Continue to increase load under the condition that no discomfort or secondary injuries occur, incorporating activities into daily life for functional strengthening.
If there is a history of osteoporosis, poor cardiopulmonary function, or other chronic diseases, thorough communication with the rehabilitation team and physicians is advised to ensure the training plan is both safe and feasible.
5. Disclaimer
This report is intended solely as a reference-based analysis of the provided imaging and clinical information. It cannot replace a face-to-face consultation or professional, individualized medical advice. The specific treatment and rehabilitation plans for the patient should be developed comprehensively based on clinical examination, surgical evaluation, and ongoing follow-up with specialist physicians.
Human Doctor Final Diagnosis
Pilomatrixoma