Charcot neuroarthropathy of the foot



Clinical History
A 56-year-old male with a history of type 2 Diabetes Mellitus presented to our institution with a painless “mass” in the left foot, associated with local swollenness, developing in the previous 2 months.
For radiological evaluation, Left Foot Radiographs and MRI were requested.
Imaging Findings
Left Foot Radiographs revealed articular bone erosions/destruction and joint distension and dislocation involving the tarsometatarsal joints (Fig. 1).
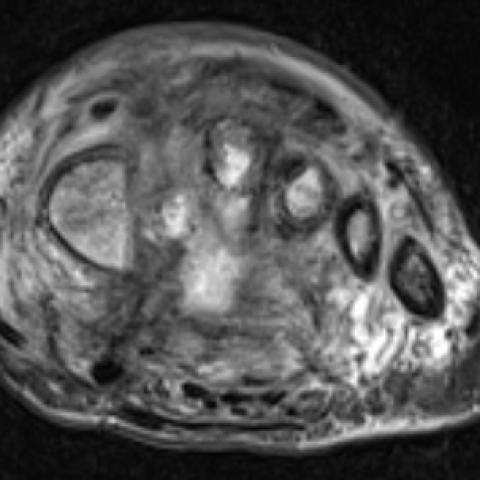
Left Foot MRI confirmed the abovementioned radiographic findings and revealed extensive bone marrow oedema involving the midfoot and metatarsals, as well as inflammatory changes in the surrounding soft tissues, including a necroinflammatory collection; the plantar subcutaneous tissue was preserved and there was no ulcer or other signs of infection. (Fig. 2).
In the context of the patient’s Diabetes Mellitus, these Imaging findings suggested Charcot neuroarthropathy of the foot.
Discussion
Charcot neuroarthropathy represents a spectrum of severely destructive osteoarticular processes associated with neurosensory deficit. [1] The most common cause of Charcot neuroarthropathy worldwide is Diabetes Mellitus; other common causes are tabes dorsalis, syringomyelia and spinal cord injury. The main pathophysiology hypothesis suggests that Charcot neuroarthropathy results from progressive inflammatory damage after a minor injury, in the context of absence of normal protective sensory feedback. [2]
One of the segments most commonly affected by Charcot neuroarthropathy is the foot, which classically occurs in the setting of Diabetes Mellitus. [1]
Charcot neuroarthropathy of the foot manifests as distortion of the articular architecture with deformity of the foot, which can lead to recurrent ulceration, cellulitis, osteomyelitis and, ultimately, amputation [2]; these features are characteristically painless [3]. Lisfranc joint is the most frequently affected joint in Charcot neuroarthropathy; involvement of the second toe with subluxation results in collapse of the foot’s longitudinal arch with “rocker-bottom” deformity, leading to increased load bearing on the cuboid and predisposing to the abovementioned consequences. [4]
Charcot neuroarthropathy may present in an atrophic - the most frequent - or a hypertrophic pattern. Both variants share joint disorganization and effusion as common Imaging features; the atrophic pattern is distinctively characterized by severe bone reabsorption and absence of/ minimal osteosclerosis, osteophytosis and bony debris; the hypertrophic pattern is distinctively characterized by osteosclerosis, osteophytosis and bony debris and absence of/ minimal bone reabsorption. [1]
Radiography is usually the first Imaging modality performed for the evaluation of Charcot neuroarthropathy, allowing overall assessment of the abovementioned imaging features. [4]
MRI plays a complementary role and allows a more sensible assessment and the detection of potential complications such as osteomyelitis and soft tissue infection. T1-weighted images reveal decreased signal intensity in the involved segments. In the initial stages, T2-weighted images depict increased signal intensity in the involved bones due to bone marrow oedema, initially in subarticular locations. In later stages, loss of demarcation of cortical outline and cortical destruction will be present. [3,4] Contrast material intravenous administration is used to better evaluate sinus tracts, abscesses, devitalized tissues, and joint or tendon involvement.
CT may be used in later-stage Charcot neuroarthropathy for better visualization of bony proliferation or for surgical planning and follow-up of immobilisation therapy. [3]
Radiologists should be familiar with the radiologic spectrum of Charcot neuroarthropathy of the foot, in order to ensure a prompt and timely diagnosis, so that the devastating consequences of a late diagnosis may be avoided. [2]
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Charcot neuroarthropathy of the foot
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Charcot neuroarthropathy of the foot - Radiography


Charcot neuroarthropathy of the foot - MRI


Charcot neuroarthropathy of the foot - MRI - Bone signal intensity changes in different MRI sequences



Medical Imaging Analysis Report
I. Radiological Findings
Based on the provided images (left foot X-ray and MRI) and medical history, the main findings include:
- Bone Alterations: Significant bony destruction and articular structural disruption observed in the tarsometatarsal (Lisfranc) joint area and nearby regions of the distal metatarsals and proximal cuneiforms; partial trabecular thinning, varying degrees of bone resorption or hypertrophic changes, and blurred cortical outlines.
- Joint Dislocation and Deformities: Evidence of joint dislocation or subluxation, with collapse of the foot arch, showing a tendency toward a “rocker-bottom” deformity.
- MRI Signal Changes:
- T1-weighted images show decreased signal in the affected bone, with disordered signal in the joint and soft tissue spaces.
- T2-weighted images suggest bone marrow edema-like high signal in the affected areas, with cortical destruction visible in certain regions.
- After contrast administration, local soft tissues and perijoint regions show enhancement. Careful evaluation for soft tissue infection or concurrent osteomyelitis is advised.
- Soft Tissue Manifestations: Noticeable local soft tissue swelling, but no significant abscess formation or large necrotic areas.
II. Potential Diagnoses
Considering the patient’s diabetic history and foot imaging findings, the following diagnoses should be taken into account:
- Charcot Neuroarthropathy (Diabetic Neuropathic Arthropathy):
- Most commonly seen in diabetic patients, caused by sensory deficits and circulatory disorders leading to ongoing microtrauma and progressive bone and joint destruction.
- Typical radiological features include disorganization and collapse of the tarsometatarsal joints, coexisting bone resorption and hypertrophic changes, subluxation or dislocation, and a “rocker-bottom” deformity.
- Osteomyelitis or Infectious Arthritis:
- In diabetic foot patients, bone destruction and soft tissue swelling can also occur, requiring differential diagnosis.
- However, classical osteomyelitis often presents with pronounced local pain, inflammatory reactions, and soft tissue abscess formation, with localized bone destruction and periosteal reaction on imaging.
- Gouty Arthritis:
- May involve foot joints, but typically presents with a history of acute painful attacks and tophus deposition.
- X-ray often shows “punched-out” erosions, while MRI reveals characteristic signals of tophi rather than widespread bone destruction.
III. Final Diagnosis
Considering the patient is 56 years old with a history of diabetes, clinical presentation (painless foot deformity), and typical imaging features (destruction and fusion at the tarsometatarsal joint, coexisting bone resorption and hypertrophy, arch collapse), the most likely diagnosis is:
- Charcot Neuroarthropathy (Diabetic Neuropathic Arthropathy).
If it is necessary to confirm whether the navicular or metatarsal subchondral bone is also infected (e.g., osteomyelitis), or to further evaluate the extent of joint damage, a bone scan or additional examinations (such as laboratory inflammatory markers or biopsy of the affected area) may be considered to definitively exclude and differentiate.
IV. Treatment Plan and Rehabilitation
- Treatment Strategies and Recommendations
- Strict Glycemic Control: Maintaining reasonable blood glucose levels helps slow neuropathic changes and further bone destruction.
- Offloading and Immobilization: Utilizing casts, removable bracing, or specialized footwear to reduce weight-bearing on the affected foot, preventing worsening deformities and promoting healing.
- Anti-Inflammatory and Anti-Infective Treatment: If there are signs of soft tissue inflammation or infection, consider appropriate use of antibiotics or related anti-inflammatory therapies.
- Surgical Intervention: In cases of severe deformity, nonunion fractures, abscess formation, or severe bone destruction, surgical correction, internal fixation, or debridement of infected foci may be required.
- Rehabilitation and Exercise Prescription (FITT-VP Principle)
During the acute phase and with significant bone destruction, priority should be given to foot protection, avoiding excessive weight-bearing and high-impact exercises. Once the condition stabilizes or after bone grafting/surgery, gradual resumption of activity can be considered.
- Frequency (F): Begin with 1–2 sessions per week of low-intensity joint mobility and muscle strengthening exercises, then increase to 3–4 sessions per week as the condition stabilizes.
- Intensity (I): Start with low-intensity activities (e.g., non-weight-bearing joint exercises or seated lower limb training). As foot stability improves, gradually introduce partial weight-bearing and light resistance training.
- Time (T): Initially 10–15 minutes per session, gradually increasing to 20–30 minutes per session. Adjust based on foot response and fatigue levels.
- Type (T):
- Early stages may include water walking, lower limb range-of-motion exercises, and core stability training to reduce foot load.
- Later stages can incorporate limited ambulation or cycling with appropriate foot orthoses, focusing on low-impact aerobic activities.
- Progression (P): Every 2–4 weeks, consider a slight increase in activity as the foot deformity stabilizes and inflammation is controlled. Monitor foot pain, skin integrity, and blood glucose levels closely.
- Volume & Personalization (VP):
- Develop an individualized regimen based on the patient’s cardiovascular fitness, blood glucose control, and comorbidities (e.g., peripheral vascular disease).
- Prevent recurrence of foot ulcers and worsening deformities. If there is reduced sensation, reinforce foot monitoring and usage of proper footwear.
Disclaimer: This report is only a preliminary analysis based on the provided images and medical history. It cannot replace an in-person consultation or professional medical advice. If you have any concerns or if symptoms worsen, please seek medical attention promptly.
Human Doctor Final Diagnosis
Charcot neuroarthropathy of the foot