Osteomyelitis of pubis



Clinical History
Pain in the left groin following a normal vaginal delivery.
Imaging Findings
A 21-year-old lady presented with pain in the pubic symphysis a year after a normal vaginal delivery. X-ray showed expansion and irregular sclerosis of the left pubic bone with some periosteal reaction. MRI and CT scan were done. She had a CT guided biopsy which grew coagulase negative Staphylococcus. She had raised inflammatory markers. She was given antibiotics with resultant response.
Discussion
Beer first described Osteitis pubis in 1924. It is usually a self limiting, non-infectious process. A variety of causes have been postulated, pregnancy, direct trauma, athlete exertion, urological manipulation and urological and gynaecological surgery. Such patients usually have progressive suprapubic pain radiating to the groin and both legs. A characteristic gait has been described which is due to abdominal muscle spasm. WBC and ESR are usually raised (but can be normal). Osteomyelitis; which is a separate condition; and osteitis pubis have similar clinical and radiological manifestations. Symptoms are suprapubic pain and tenderness. Pain increases on ambulation. Bone destruction is more pronounced with osteomyelitis than with osteitis pubis. Less then 10% of cases of osteomyelitis occur in the pelvis with pubis the least affected. Two cases of osteomyelitis of pubis following normal vaginal delivery have been reported before. In both osteomyelitis and osteitis pubis, x-ray of the pubic bone shows bone rarefaction and erosion. There may be separation of symphysis. MRI is useful in the early stages, demonstrating marrow oedema. The abnormal marrow has a low T1W and a high T2W signal. Additional abnormalities in osteomyelitis are cortical erosion or perforation, periosteal reaction, abscess, sequestrae and sinus tracts. MRI is useful in ruling out active marrow involvement, localising pus collections in chronic osteomyelitis and in separating cellulitis alone from cellulitis with osteomyelitis. Fat saturation and contrast-enhanced sequences are usually used. STIR sequence is particularly useful. Brodie’s abscess is seen better after contrast, sequestrae are low to intermediate on the T1W and T2W and show no enhancement. Burns and Gregory proposed that the diagnosis of osteomyelitis requires the presence of radiological changes and histologic finding of infection of both bone and bone marrow. This may mean blood culture and/or bone aspiration or biopsy. Hoymes reported that Staphylococcus aureus is found in 60% of cases and gram negative bacteria in 40%. For suspected osteomyelitis, treatment with intravenous antibiotics followed by oral antibiotics for an appropriate duration is recommended. Surgery may be required in certain cases.
Differential Diagnosis List
Final Diagnosis
Osteomyelitis of pubic bone.
Liscense
Figures
X-Ray Pubic symphysis

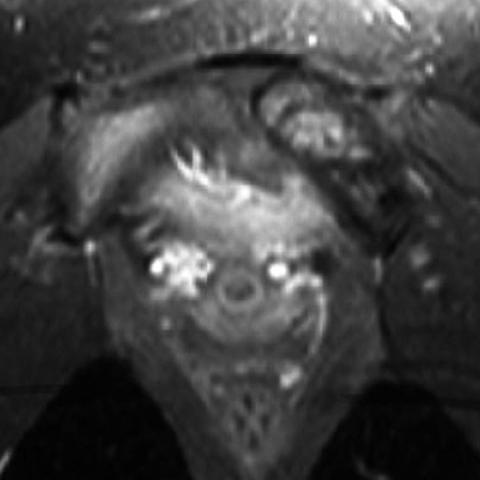
MRI Pelvis


Plain film after Treatment

MRI Pelvis

1. Radiological Findings
Based on the provided pelvic X-ray and MRI sequence images, there is an abnormal density or signal in the region of the pubic symphysis. Some areas show mild osteoporosis and marginal bone destruction. On T1-weighted images, local signal reduction is observed, while T2-weighted or STIR sequences show high signal changes, suggesting local edema or inflammation. If there is notable enhancement after contrast administration, attention should be paid to whether there is cortical bone or soft tissue destruction or the possibility of an abscess.
Overall, the bone abnormalities are primarily located at the pubic symphysis, either bilaterally symmetrical or approximately symmetrical. A mild change in the pubic symphysis space may be present. Considering the clinical symptoms (left inguinal pain postpartum) and occasional elevated inflammatory indicators, an inflammatory or infectious lesion should be considered.
2. Potential Diagnoses
- Osteitis Pubis
- Commonly seen postpartum, in athletes, or after pelvic surgery. It is a non-infectious, inflammatory condition leading to pain in the pubic symphysis that can radiate to the groin or medial thigh.
- Radiologically, it may show osteoporosis at the pubic symphysis, marginal erosions, and an irregular joint space, but the degree of destruction is usually relatively mild.
- Osteomyelitis of the Pubis
- May be caused by bacterial pathogens (e.g., Staphylococcus aureus), presenting with symptoms similar to osteitis pubis, but often with more pronounced local or systemic symptoms such as high fever and significantly elevated white blood cell counts and inflammatory markers.
- Imaging findings can include noticeable bone destruction, cortical erosion, soft tissue abscess formation, or sequestra.
- It is extremely rare in the postpartum setting, but some cases have been reported in the literature.
The radiographic and MRI findings for both conditions can show destructive changes or irregularities at the pubic symphysis, making clinical and laboratory tests (e.g., blood cultures, bone biopsy) critical in the differential diagnosis.
3. Final Diagnosis
Taking into account the postpartum context, the characteristic symptoms (pain in the pubic symphysis/groin), and the lack of extensive bone destruction or obvious abscess on imaging, the current conclusion leans toward Osteitis Pubis. However, since osteomyelitis of the pubis can present similarly in early stages, if the patient’s inflammatory markers remain elevated or clinical pain worsens, the possibility of osteomyelitis must not be ruled out. Further investigations such as blood culture and/or bone biopsy should be considered to confirm or exclude infection.
4. Treatment Plan and Rehabilitation Program
4.1 Treatment Strategy
- Conservative Treatment: For suspected or confirmed osteitis pubis, conservative management is typically first-line, including anti-inflammatory and analgesic medications (e.g., NSAIDs) to relieve pain and inflammation. Adjunct local physical therapy (e.g., warm compresses, ultrasound therapy) may also be considered as needed.
- Antibiotic Therapy: If osteomyelitis of the pubis is strongly suspected or confirmed, prompt and effective antibiotic treatment is necessary (initially intravenous, then oral). Antibiotic selection is based on blood culture and pathogen identification, and the treatment course may be prolonged (typically at least 4-6 weeks).
- Surgical Intervention: In cases of confirmed osteomyelitis complicated by abscess formation or sequestra, or if conservative treatment fails, surgical debridement and drainage, and even sequestrectomy, should be considered.
4.2 Rehabilitation and Exercise Prescription
After acute pain subsides or infection is effectively controlled, a rehabilitation schedule can be gradually introduced, adhering to the FITT-VP principle (Frequency, Intensity, Time, Type, Volume, Progression):
- Early Stage (after acute pain relief)
- Frequency: 2-3 sessions per week, avoiding excessive fatigue.
- Intensity: Low-intensity exercises targeting the stabilization of the pelvis and core muscles, such as supine leg raises and bridge exercises.
- Time: 10-15 minutes each session; discontinue if pain occurs.
- Type: Core stabilization and low-resistance training around the hip joint.
- Intermediate Stage (after significant reduction in pain and inflammation)
- Frequency: 3-4 sessions per week, with appropriate rest intervals.
- Intensity: Moderate-intensity resistance training and low-impact aerobic exercise, such as brisk walking over short distances or cycling with low resistance.
- Time: 20-30 minutes per session, extend as tolerated.
- Type: Continued enhancement of core strength and multi-joint coordination, as well as lower limb muscle strengthening.
- Late Stage (functional recovery and strengthening)
- Frequency: 4-5 sessions per week, possibly including cross-training.
- Intensity: Gradually increase resistance or speed, emphasizing higher levels of strength and endurance.
- Time: 30-40 minutes per session, or adjusted according to individual recovery.
- Type: May resume appropriate running, jumping, and other weight-bearing exercises while continually monitoring the pubic symphysis for adverse reactions.
Throughout the rehabilitation process, it is essential to closely monitor changes in pain and inflammatory markers. If notable exacerbation of pain or local redness and swelling occurs, prompt re-evaluation and imaging review should be performed.
Disclaimer
This report is based on the available data for reference and does not replace face-to-face consultation or the opinion of a professional physician. Specific treatment plans should be determined by the attending physician after a comprehensive evaluation of the patient’s actual condition.
Human Doctor Final Diagnosis
Osteomyelitis of pubic bone.