Parosteal Lipoma


Clinical History
CT and MRI are the methods of choice for diagnosis of osseous and non osseous lipomas.
Imaging Findings
The patient consulted for a painless mass at the left thigh occurring after a sports injury 20 years ago. Besides a perimetric difference of 10 cm at the superior aspect of the thigh clinical examination revealed no further abnormalities.
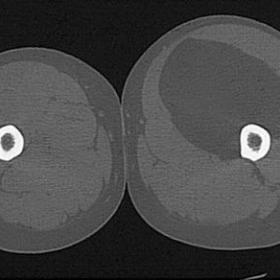
CT of both thighs shows an exostotic lesion at the medial aspect of the left femur surrounded by a large, well-circumscribed fatty mass (-80 HU) within or displacing the left quadriceps muscle.
Arteriography of the left femoral artery (non subtracted and subtracted image) demonstrates major branches of the femoral artery displaced by the large mass, without obvious pathological vessels.
Radiography of the left femur shows a large soft tissue mass around an exostotic-like lesion at the medial border of the left femur. There is no continuity between the medullary bone of the femoral shaft and of the exostosis.
The radiological diagnosis of parosteal lipoma was confirmed by the (incomplete) surgical resection and by the pathological examination of the specimen (intramuscular lipoma with osseous and chondroid metaplastic components adhesive to the femoral bone, without signs of malignant degeneration).
Discussion
Lipoma is one of the most common soft tissue tumors. Its osseous localization s rather unusual (0.3%). Three types have been described in respect to their relationship with bony structures i.e. intraosseous, cortical or parosteal. The lesion is always solitary and preferably affects the metaphyses of the long bones (femur, tibia and humerus). The tumor is mostly asymptomatic and does not have any preference according to age or sex. It presents as a slowly growing mass with an average of eight to ten years of evolution. Clinical symptoms are related to compression of adjacent neurovascular and muscular structures and depend on the size and location of the lesions. CT and MRI are the methods of choice for diagnosis of osseous and non osseous lipomas. On CT they present with a low attenuation (-20-80 HU), on MR with a high signal intensity on T1-WI, an intermediate SI on T2-WI and they loose signal on fat suppressed sequences. They do not enhance after IV Gadolinium injection. Bone reactive changes resemble osteochondromatous exostosis but they lack contiguity of adjacent cortex and medulla as described in osteochondromas. Differential diagnosis with low grade liposarcoma can be difficult but neither primary parosteal liposarcoma nor degenerated benign parosteal liposarcoma have been described in literature.
Differential Diagnosis List
Final Diagnosis
Parosteal lipoma
Liscense
Figures
CT of both thighs


Arteriography of the left femoral artery


Radiography of the left femur

1. Imaging Findings
The patient is a 30-year-old male. CT scans reveal a lesion with fat-like density in the soft tissue of the right thigh, with CT values approximately (-20 ~ -80 HU), consistent with the characteristics of adipose tissue. The lesion has relatively clear boundaries. Reactive bone proliferation adjacent to the bone cortex is noted locally, but there is no obvious continuity between the lesion and the bone cortex or the medullary cavity. MRI (if obtained) would likely show high signal intensity on T1-weighted images and moderate-to-high signal intensity on T2-weighted images, with marked signal reduction on fat-suppressed sequences. After contrast enhancement, no significant enhancement is seen within the lesion. The imaging appearances match fat signal characteristics, accompanied by local bony reaction similar to an exostosis. However, unlike a true osseous outgrowth (e.g., osteochondroma), there is no continuity of the lesion’s cortex and medullary cavity with that of the host bone.
2. Potential Diagnosis
- Parosteal Lipoma: A rare form of lipoma attached to the periosteum, often accompanied by reactive bone formation. Imaging typically shows a fat-density/signal lesion with possible formation resembling an exostosis around or within it.
- Osteochondroma: A common benign bone outgrowth. Key features include continuity of the outgrowth’s cortex and medullary cavity with the parent bone. In this case, there is no obvious continuity, making this diagnosis less likely.
- Low-grade Liposarcoma: Can appear similar to a lipoma on imaging, but may have atypical components or thickened soft-tissue elements. Some degree of enhancement may be observed. There are currently no clear signs suggesting malignant transformation in this case.
3. Final Diagnosis
Taking into account the patient’s age, clinical presentation (usually slow growth and possible local compression symptoms), imaging characteristics (fat-density lesion with local bone reaction but no continuity with the medullary cavity), and the literature indicating that such occurrences, though rare, have been reported, the most likely diagnosis is:
Parosteal Lipoma.
If there is still uncertainty about the nature of the lesion, a biopsy or follow-up imaging may be considered to rule out the possibility of a low-grade liposarcoma.
4. Treatment Plan and Rehabilitation Plan
Treatment Strategy:
- If there are no significant symptoms or signs of compression, close monitoring with regular imaging studies can be chosen to observe any changes in lesion size.
- If pain, neurovascular compression, functional impairment, or a larger lesion with malignant potential are present, complete surgical excision should be considered. Careful protection of the nearby nerves and vessels is crucial during surgery.
- Recurrence is very rare after complete resection of a benign lipoma.
Rehabilitation and Exercise Prescription Recommendations (FITT-VP principle):
- Frequency: In early postoperative stages, low-intensity activities can begin 2–3 times per week, gradually increasing to 3–5 times per week depending on recovery.
- Intensity: Start with light to moderate intensity, such as walking, simple lower limb joint movements, and light resistance exercises. Avoid excessive stretching or impact at the surgical site.
- Time: 15–30 minutes per session initially, gradually increasing to 30–45 minutes based on patient endurance and wound healing.
- Type: Low-impact aerobic exercises such as brisk walking or stationary cycling. Add light-to-moderate resistance training (e.g., resistance band workouts) to improve lower limb strength and stability.
- Volume & Progression: Increase exercise duration and resistance levels as the incision and soft tissues heal. If any pain or discomfort arises, adjust the training plan and seek medical evaluation.
Throughout rehabilitation, closely monitor the surgical area for healing status and potential neurovascular symptoms. If severe pain, swelling, or numbness occurs, seek immediate medical attention. For patients with weaker bone structures or lower overall fitness, exercise plans should be more conservative and progressive, ideally under the guidance of a professional rehabilitation therapist or orthopedic specialist.
5. Disclaimer
This report serves only as a reference analysis based on existing data and does not replace an in-person consultation or professional medical advice. Diagnosis and treatment plans should be formulated by orthopedic and related specialists after a comprehensive evaluation of the patient’s specific condition.
Human Doctor Final Diagnosis
Parosteal lipoma