Os Omovertebrale: A congenital deformity



Clinical History
A 7-year-old female patient presented with restricted left-sided shoulder and arm movement. On examination, there were asymmetrically shoulders with left shoulder deformity seen. In addition, Limited neck movements were seen on the affected sides. Blood reports show mild microcytic hypochromic anaemia.
Imaging Findings
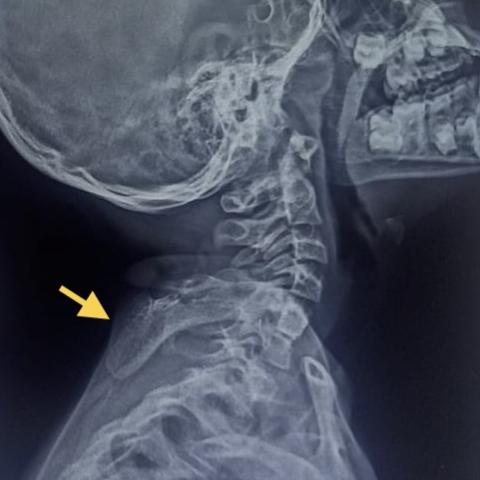
Frontal and lateral radiographs of the cervical spine showed Spina bifilar at C3, C4 and C5 vertebral levels with a bony density overlapping over the left lamina and pedicels. Broad-based skeletal density was seen extending posteriorly From posterior cervical elements into the posterior cervical soft tissue.AP radiograph of Left shoulder shows mild scoliosis with spina bifida at previously described levels with fan-shaped bony density extending laterally towards a superomedial aspect of the scapula.CT bone window axial cuts show a skeletal density in close AP proximity of left lamina, transverse and spinous process of C5 with mild sclerosis. The accessory bone joins laterally at the superomedial aspect of the left scapula.CT 3D constructions showed a similar bony bridge between the lower cervical spine and scapula with another small bony projection from the spinous process of C6.T1WI MRI axial showed similar skeletal density with no visualization of left trapezius and asymmetry of left lavatory scapulae and semi spinal is muscles.
Discussion
Os omovetebrale is an osseofibrocatilagenous connection between the lower cervical or upper dorsal spine and the medial border of the scapula. Most commonly found at the level of C4-C7 and rarely at T1. Most cases described are children; adults can also present with omovertebral bone and features of compressive myelopathy. The most accepted theory in connection with the origin of bone is that the bone is the original scapular element which becomes secondarily fused to the spine [1]. The four-tier classification system [2] identifies the morphological characteristics and helps decision-making.
Proposed classification system for the vertebral anomaly-
Type I-Fibrous
Type II-Osseous-Fibrous
Type III-Osseo-Cartilagenous
Type IV-Osseous (True)
Sprengel deformity is a rare congenital deformity of children, which is associated with a hypoplastic, medially rotated, triangular-shaped scapula with restricted abduction and flexion of the involved shoulder. The scapula is elevated with scapular winging. Incidence is more in female children with M: F=1:3.This condition may occur bilaterally in 10-30% of cases. Interruption of embryonic subclavian blood supply at the level of subclavian, internal thoracic or supra-scapular artery and failure of caudal migration of shoulder to its normal position is considered the aetiology [3,4]. In addition, this deformity is associated with muscle atrophy of the pectoral girdle resulting in disfigurement [5].
One-third of cases of Sprengel's shoulder is associated with Klippel Feil deformity. In addition, congenital scoliosis is often seen. Other uncommon associations are diastematomyelia and renal disease[1]. Omovertebral connection between the cervical spine (C4-C7) and medial angle of the scapula is present in 30-50% of cases. This connection may be fibrous or osseous [6]. Occasionally it may be bilateral.
Diagnosis is often clinical. Plain Radiographs are used as a screening method to evaluate the bony bar; however, fibrous connections require assessment with CT/MRI.CT 3D reconstructions are especially helpful in preoperative planning.MRI is indicated in compressive cervical myelopathy or a review of ipsilateral brachial plexus.
Functional deformities and cosmetic concerns indicate operative treatment (abduction< 110-120 degrees). Surgery is best performed in 3-8 yrs because of the risk of nerve entrapment after age 8. The surgical outcome is significantly favourable, especially in cases with compressive myelopathy. In the absence of shoulder dysfunction, observation is the treatment of choice[1]
Teaching points
Imaging plays a distinct role in management by identifying the morphology of omovertebral bone based on different types, especially when it is not a part of Sprengel scapula.
Differential Diagnosis List
Final Diagnosis
Sprengel shoulder with spinal dysraphism
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures







Medical Imaging Analysis Report
I. Radiological Findings
This patient is a 7-year-old female, presenting with restricted mobility of the left shoulder joint and upper limb. On examination, there is visible asymmetry and deformity of the left shoulder, accompanied by limited neck movement on the same side. Based on the provided X-ray, CT, and MRI images, the main radiological features are as follows:
- An abnormal bony/fibrous connection (indicated by the yellow arrow) can be seen between the cervical vertebrae and the medial border of the left scapula. CT 3D reconstruction clearly illustrates this “band-like” structure that extends from the lower cervical spine (approximately C5-C6) to the medial border of the scapula.
- The left scapula is positioned higher, shows a rotated, slightly smaller, and triangular shape consistent with Sprengel’s deformity.
- A “winged” appearance of the shoulder is noted, and there are signs of underdevelopment of the shoulder girdle musculature.
- No obvious segmental defects of the vertebral bodies were observed, but congenital variations in the relevant structures are visible.
- On MRI axial images, the soft tissues around the scapula appear relatively atrophic, corresponding to the abnormal scapular position.
II. Potential Diagnoses
Based on the above radiological findings and the patient’s clinical characteristics, the following potential diagnoses may be considered:
- Sprengel’s Deformity (Congenital High Scapula) with Omovertebral Bone
This condition is a rare congenital deformity in children, characterized by an elevated, smaller scapula and restricted shoulder movement. Approximately 30–50% of Sprengel’s deformities are associated with a fibrous or bony connection from the cervical or upper thoracic vertebrae to the medial border of the scapula (known as the omovertebral bone). The images in this case show these features, which is highly indicative of this diagnosis. - Other Congenital Shoulder Girdle Deformities
Such as abnormal development of the shoulder or clavicle, although most do not exhibit the distinct bony connection between the cervical vertebrae and scapula. Usually, only underdevelopment of the clavicle or acromion is observed, which differs from the presentation in this case.
III. Final Diagnosis
Considering the patient’s age, symptoms (restricted mobility and abnormal appearance of the left shoulder), radiological findings (elevated and rotated scapula, abnormal bony/fibrous connection from the cervical spine to the medial border of the scapula), and typical forms reported in the literature, the most likely diagnosis is:
“Sprengel’s Deformity with Omovertebral Bone”
This diagnosis adequately explains the patient’s restricted shoulder movement and deformity. Mild anemia noted in blood tests does not affect this skeletal diagnosis.
IV. Treatment and Rehabilitation Plan
For pediatric patients with Sprengel’s deformity combined with omovertebral bone, the treatment goals include improving shoulder joint function, reducing the deformity, and preventing further muscle and skeletal developmental abnormalities. The main treatment strategies are as follows:
- Conservative Treatment
- If the child’s shoulder function is acceptable, with no significant pain or neurological symptoms, conservative management can be considered first.
- This includes physical therapy and exercises to strengthen the shoulder joint and shoulder girdle muscles (such as passive stretching, active range-of-motion exercises, scapular stabilization training, etc.).
- Regular monitoring of skeletal growth and shoulder range of motion is advised to assess the need for further surgical intervention.
- Surgical Treatment
- If marked limitation in shoulder abduction (less than 110–120°) or significant impact on appearance and daily function is present, surgery is recommended between ages 3–8 to achieve better postoperative function and cosmesis.
- Surgery may include removal of the omovertebral bone and related soft tissue release, or even repositioning of the scapula.
- Comprehensive preoperative imaging (especially CT 3D reconstruction and MRI) is crucial in planning the surgical approach.
Rehabilitation and Exercise Prescription
Regardless of whether conservative or surgical treatment is chosen, rehabilitation therapy is essential. It should follow the FITT–VP principle (Frequency, Intensity, Time, Type, Progression, Volume, and Individualization) to incorporate a progressive and safe regimen, for example:
- Training Frequency (F): 3–5 times a week.
- Training Intensity (I): Start with low-intensity, short-duration activities, such as active/passive range-of-motion exercises for the shoulder joint, each lasting 5–10 minutes. Intensity can be gradually increased as range of motion and muscle strength improve.
- Training Time (T): Based on the child’s tolerance, 15–20 minutes per session is recommended, divided into multiple sets. Postoperative rehabilitation should follow a gradual increase under medical supervision.
- Training Type (T):
- Exercises to improve shoulder flexion, extension, abduction, and internal/external rotation range of motion.
- Strengthening exercises (isometric and isotonic) for the shoulder girdle muscles (trapezius, middle and lower rhomboids, etc.) to enhance scapular stability.
- Elastic band training may be introduced cautiously, avoiding painful ranges.
- Progression (P) and Volume (V): Gradually increase the number and difficulty of exercises based on the child’s response, moving from passive stretching to active resistance training while avoiding excessive strain that could lead to soft tissue injury.
- Individualization (I): If the child has other underlying conditions, such as anemia or reduced cardiopulmonary function, training volume and intensity should be appropriately adjusted under medical supervision.
In summary, rehabilitation should be carried out under the guidance of professional rehabilitation or orthopedic specialists to ensure functional improvements without causing secondary injury.
Disclaimer: This report provides a reference-based medical analysis derived from existing information and does not replace in-person consultation or professional face-to-face medical evaluation and treatment. A specific treatment plan should be determined based on actual clinical conditions under the guidance of a qualified physician.
Human Doctor Final Diagnosis
Sprengel shoulder with spinal dysraphism