


The patient presented with a five-week history of increasing pain in the right elbow. Physical examination showed tumefaction of the proximal end of the ulna. Plain radiographs, CT and MRI were performed.
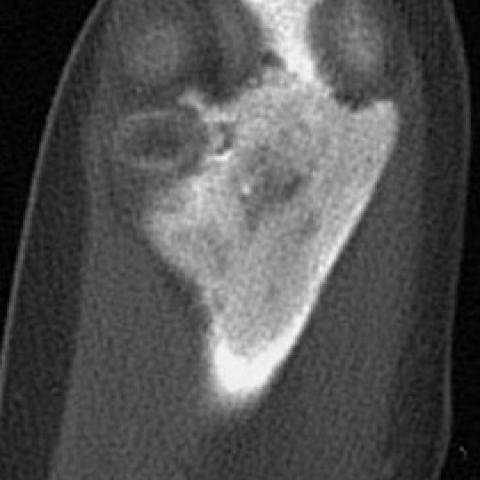
The patient presented with a five-week history of increasing pain in the right elbow. Physical examination showed tumefaction of the proximal end of the ulna. The patient had no fever, chills, weight loss or prior trauma. Laboratory tests were unremarkable. Plain radiographs (Fig. 1), CT (Fig. 2) and MRI (Fig. 3) were performed. Final diagnosis was established by trephine biopsy.
Skeletal fibrous dysplasia is a developmental anomaly, typically encountered in adolescents and young adults, in which normal bone marrow is replaced by fibro-osseous tissue (1).
Radiographs show a well-defined medullary lesion, usually with thick sclerotic borders. It can be moderately expansive but the cortex is intact and there is usually no periosteal new bone formation. Depending on the amount of woven bone present and the extent to which it is mineralised, the lesion may have a radiolucent, ground-glass, or even sclerotic appearance. The disease may affect a single bone (monostotic fibrous dysplasia), or many bones (polyostotic fibrous dysplasia). Any bone in the skeleton may be affected and lesions may involve only a small segment of a bone or extend along most or all of a long bone. In the long bones, it usually arises at the metaphysis, but can occur at any location, including the epiphysis before and after closure of the growth plate (2,3).
The present case showed an extensive proximal ulnar epiphyseal involvement, with dysplastic fibro-osseous tissue reaching the joint surface over a wide area. The epiphyseal involvement was associated with multiple erosions of the articular cortex and some well-defined radiolucent foci in subchondral bone, which were evident on CT scans but were unapparent on plain radiography. To our knowledge, these findings have not been previously described in association with fibrous dysplasia. We speculate that these findings might represent osteonecrotic changes secondary to increasing marrow pressure caused by the growth of the dysplastic fibrous tissue. A superimposed septic arthritis may be ruled out in the absence of joint space narrowing and disease in the other side of the joint.
Monostotic fibrous dysplasia





Based on the provided X-ray, CT, and MRI images, a large area of abnormality in the right proximal ulna (near the elbow joint) is observed, specifically characterized by:
The overall imaging characteristics indicate that the lesion is primarily related to a fibrous-osseous proliferative process within the bone, with a wide extent. Involvement of the physis and its proximity to the articular surface is relatively rare.
Combining the patient’s age of 16, clinical presentation (right elbow pain for 5 weeks without a clear history of trauma), and the imaging findings, the main differential diagnoses are as follows:
Considering the patient’s age, symptoms, and imaging features, “Fibrous Dysplasia (Fibro-Osseous Dysplasia)” best matches the overall presentation. The ground-glass appearance, relatively distinct borders, lack of significant periosteal reaction, and the wide lesion extent approaching the articular surface are all consistent with monostotic fibrous dysplasia. Although involvement of the epiphysis and close proximity to the joint surface is uncommon, the lesion’s density characteristics and clinical course support this diagnosis. A biopsy could be performed for further confirmation if needed.
For monostotic fibrous dysplasia, clinical management typically depends on symptom severity and the stability of the bony structure:
Rehabilitation/Exercise Prescription (FITT-VP Principles):
During rehabilitation, pay close attention to pain, swelling, and the structural integrity of the bone. In cases of fragile bone or a high risk of pathological fracture, carefully regulate exercise intensity and joint loading.
This report is based on the available imaging data and clinical information for reference only, and should not be considered a substitute for an in-person consultation or professional medical advice. If any questions or changes in condition arise, please seek further evaluation and treatment at a qualified medical institution.
Monostotic fibrous dysplasia