Osteoid osteoma of the scapula: two cases studied with CT and MR imaging



Clinical History
Two patients complaining of a lengthy history of pain on the scapula. The pain was continuous during the day with no night exacerbation. The plain X-rays were normal in each case.
Imaging Findings
The first patient, a right-handed manual worker, complained of a 2-year pain over the left shoulder area, not associated with trauma. His general practitioner suggested non-steroidal anti-inflammatory medication along with physiotherapy, but there was no improvement. Five months later, the patient was referred to an orthopaedic surgeon because of reduced motility of the shoulder joint and increasing pain. The first clinical diagnosis was impingement syndrome. The plain radiograph was normal. CT showed a lytic lesion in the scapular neck (Fig. 1a). MR imaging showed a lesion of intermediate signal intensity on T2-weighted images, along with intra-articular fluid (Fig. 1b). The scintigram showed an increased uptake in the blood pool phase (Fig. 1c). The patient underwent surgical excision and has since remained asymptomatic for 2 years.
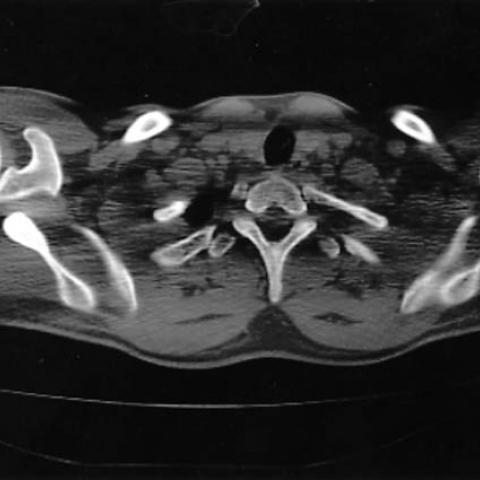
The second patient complained of a 4-year pain in the right shoulder area, not associated with a traumatic event. The pain was continuous during the day and there was no night exacerbation. The plain radiograph was normal. The orthopaedic surgeon suggested a CT scan. The 5mm thick axial scan showed diffuse osteosclerosis (Fig. 2a) and a 1.5mm bone algorithm examination showed a lytic lesion with a central nidus associated with periosteal reaction (Fig. 2b). The patient underwent surgical excision and has since remained asymptomatic for 13 months.
Discussion
Osteoid osteomas are benign bone tumours presenting radiologically as lytic lesions with or without sclerotic nidus. The lesion is associated with a typical sclerotic periosteal reaction. The clinical features of aching pain worsening at night and relieved with aspirin are typical. However, there are cases that may present atypically as a less painful synovitis. In cases where non-typical clinical features are associated with rare locations, the diagnosis may be delayed for years (1). The cases presented here did not present with typical clinical symptoms, but the histology of the excised lesions showed osteoid osteoma.
The scapula is a rare location for osteoid osteomas with fewer than 20 cases being reported in the literature (2-4). Plain radiographs are not very helpful in identifying the lesion because of overlapping structures. Hot scintigraphy and CT with bone algorithm at the area of interest are the suggested methods for diagnosing osteoid osteomas. MR imaging can suggest the diagnosis but it is not the method of choice. Treatment of choice used to be complete surgical excision but since a substantial piece of bone is usually resected, complications such as hematoma, infection, and fracture may result. CT-guided percutaneous thermocoagulation is a minimally invasive, safe, and effective procedure for treatment of osteoid osteoma, including spinal lesions, with a success rate of over 76%(5).
Differential Diagnosis List
Final Diagnosis
Osteoid osteoma of the scapula
Liscense
Figures
Scapular osteoid osteoma: case 1



Scapular osteoid osteoma: case 2

Medical Imaging Analysis Report
I. Radiological Findings
Based on the provided CT, MRI, and bone scan data, a small localized bony lesion is noted in the scapular region:
- CT Images: Slightly increased density or a low-density lucent area (suspected “lesion center”) is observed near the scapula, with mild surrounding sclerosis and bone reaction.
- MRI Images: A certain degree of signal alteration is visible at the lesion site. On T1-weighted images, the lesion may show low to intermediate signal, while on T2-weighted images, it may present high signal. There is no obvious swelling or abnormal enhancement in the surrounding soft tissues.
- Bone Scan (Bone Scintigraphy): The “hot spot” at the lesion site indicates high radioactive uptake, suggesting active bone metabolism.
- Conventional X-ray: Due to overlapping structures of the scapula, plain radiography has limited diagnostic value and shows no significant abnormalities.
II. Potential Diagnoses
Taking into account the clinical symptoms (scapular pain persisting during the day without typical nocturnal exacerbation, previously normal X-rays) and the imaging findings, the following potential diagnoses are considered:
- Osteoid Osteoma: Typically presents with nighttime worsening and sensitivity to NSAIDs, although atypical cases exist. On imaging, one may see a small sclerotic or lucent nidus with a surrounding sclerotic rim. Bone scan shows focal high uptake.
- Osteoblastoma: Similar to osteoid osteoma but generally presents with a larger lesion; clinical pain can also be atypical. In addition, MRI more commonly reveals significant bone destruction or a soft tissue reaction.
- Benign Cystic Lesion of the Scapula (e.g., simple bone cyst): Usually appears as a cystic lucent area with minimal sclerotic reaction. Persistent pain is uncommon unless a pathological fracture occurs.
- Fibro-Osseous Lesion (e.g., fibrous dysplasia): Rare in the scapula, but on imaging may show a “mixed density” or “ground glass” appearance.
III. Final Diagnosis
Based on the pathological findings after surgical resection indicating osteoid osteoma, combined with the patient’s clinical presentation and imaging characteristics, the final diagnosis is: Osteoid Osteoma (Scapula).
Although the patient did not exhibit classic nighttime exacerbation or dramatic relief with aspirin, atypical presentations are not uncommon. Effective auxiliary diagnostic approaches include CT localization and bone scan.
IV. Treatment Plan and Rehabilitation
1. Treatment Strategies
- Surgical Resection/Curettage: The traditional approach involves complete removal of the lesion, including the osteoma and surrounding sclerotic rim; however, one must consider the potential for bleeding, infection, or structural damage leading to functional impairment.
- CT-Guided Radiofrequency Ablation: A minimally invasive procedure utilizing percutaneous thermal ablation under CT guidance, offering a high success rate and avoiding extensive bone resection.
- Medication for Symptomatic Relief: Short-term use of NSAIDs can help alleviate pain. In cases of chronic pain, an individualized analgesic regimen is recommended.
2. Rehabilitation and Exercise Prescription
Following surgery or minimally invasive treatment, patients may benefit from the following exercise prescription principles (FITT-VP):
- Type: Emphasize protecting shoulder joint and scapular stability, such as mild shoulder range-of-motion exercises and small-range shoulder girdle strengthening with resistance. Progressively incorporate resistance bands and multi-angle isometric exercises.
- Frequency: 3–5 times per week, with gradual escalation based on postoperative pain and tolerance.
- Intensity: Begin with low-intensity activity, avoiding large-amplitude rotations or heavy lifting. As recovery advances, gradually increase resistance or introduce higher training loads.
- Time: Start with 15–20 minutes per session in the early stage, then progressively extend to 30 minutes or longer as tolerated.
- Mode: Combine range-of-motion exercises, low-resistance muscle strengthening, and posture correction training. Proper technique should be emphasized.
- Progression: Once pain is significantly relieved and range-of-motion is nearly restored, introduce moderate to slightly higher intensity shoulder trainings (e.g., swimming strokes, low-intensity barbell exercises) to assist in comprehensive recovery of bone and soft tissue function.
Throughout the rehabilitation process, pain intensity and shoulder mobility should be closely monitored. If symptoms worsen, seek prompt medical evaluation. Patients with fragile bone conditions or other comorbidities should engage in these exercises under the guidance of a specialist or physical therapist.
Disclaimer
This report is based solely on the provided imaging and available information for initial analysis and does not replace in-person clinical evaluation. If you have any questions or if your condition changes, please seek professional medical advice promptly for appropriate assessment and treatment.
Human Doctor Final Diagnosis
Osteoid osteoma of the scapula