Brown tumours simulating neoplasia



Clinical History
The patient was admitted with a fracture of the left upper arm after a minor fall. Plain radiography and MRI revealed an expansile benign lytic lesion in the proximal left humerus. One month after conservative treatment, the patient was readmitted because of persistent pain not responding to analgesics. The imaging procedures suggested an aggressive lesion. A bone scintigram showed multiple lesions. The complete biochemical workout revealed increased serum calcium (3.46mmol/l).
Imaging Findings
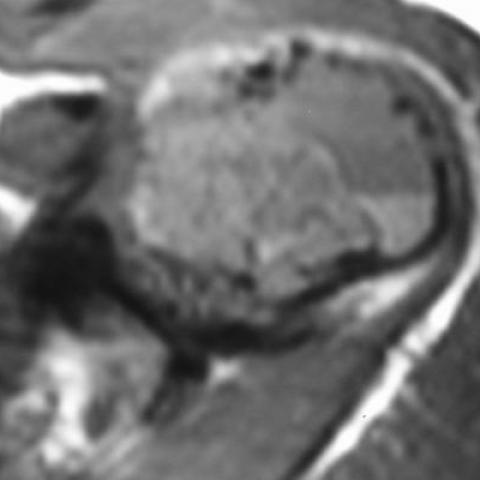
The patient was admitted to hospital because of a fracture of the left upper arm after a minor fall. The clinical examination and her medical history were unremarkable. The plain radiograph (Fig. 1a) revealed an expansile lytic lesion in the proximal left humerus. An MRI was requested for further investigation. This revealed on both T1-weighted spin echo (Fig. 1b) and T2-weighted TSE (Fig. 1c) fluid-fluid levels with haemorrhagic components. A benign tumour was diagnosed and conservative treatment was suggested.
One month later, the patient was again admitted to hospital because of persistent pain not responding to analgesics. A plain radiograph showed an aggressive expansile lytic lesion of the proximal humeral metadiaphysis (Fig. 2) and a pathological fracture. Axial CT showed a lytic lesion involving the cortex and the medulla (Fig. 3). On MRI scan, T2-weighted TSE images with fat-suppression showed increased signal intensity in the humerus and the surrounding soft-tissues (Fig. 4a). T1-weighted spin echo (Fig. 4b) and enhanced T1-weighted spin echo with fat suppression (Fig. 4c) showed that in a one-month period the lesion had changed, exhibiting intense contrast enhancement and soft tissue extension. These appearances were suggestive of an aggressive lesion. A bone scintigram showed multiple lesions at the left proximal humerus, left proximal femur, left tibia and right iliac bone. An axial CT scan of the pelvis showed multiple lytic lesions involving the cortex and the medulla (Fig. 5), with erosion of the outer cortical bone in one of them. The complete biochemical workout revealed increased serum calcium (3.46mmol/l).
Discussion
The original radiological diagnosis (Fig. 1) was aneurysmal bone cyst (ABC) because the lesion was expansile, well defined and showed fluid-fluid levels with haemorrhage. One month later, the radiological findings (Figs 2-4) suggested an aggressive lesion, probably telangiectatic osteosarcoma associated with ABC. An open biopsy was performed and the complete histological study showed a high grade giant cell tumour (GCT). After the CT scan and the bone scan (Fig. 5), revealed multiple lesions, a diagnosis of multiple GCT was considered and the patient was scheduled for surgery of the humeral lesion. A review of the original histology in another centre suggested a differential diagnosis of solid ABC and GCT.
The preoperative biochemical analysis showed elevated serum calcium and a subsequent PTH measurement showed 1057 (normal 10-60). A diagnosis of primary hyperparathyroidism was established and the patient underwent surgery. A 5.3g parathyroid ademona was removed. The serum calcium decreased and follow-up radiographs of all lytic lesions showed progressive healing.
The commonest lesion showing fluid-fluid levels with haemorrhage on CT and/or MRI is primary or secondary ABC (1,2). The presence of fluid-fluid levels in an osseous lesion is not pathognomonic of a specific lesion (3). The association of fluid-fluid levels and brown tumours has recently been reported (4). Although not previously reported, it is not unexpected to find fluid-fluid levels in brown tumours since these tumours often contain haemorrhage (4).
Differential Diagnosis List
Final Diagnosis
Brown tumours
Liscense
Figures
Lytic lesion of the left humerus


Radiograph obtained one month after initial presentation

CT scan of the left humerus

MR imaging on second admission



CT scan of the pelvis

Medical Imaging Analysis Report
I. Imaging Findings
1. A clearly visible expansile lytic lesion is noted in the proximal left humerus, with relatively well-defined margins.
2. MRI shows “fluid-fluid levels” within the lesion, suggesting cystic or hemorrhagic components.
3. Follow-up imaging suggests the lesion has become more “aggressive,” possibly affecting adjacent tissue to some extent, but there is currently no clear evidence of extensive soft tissue invasion.
4. Bone scan indicates multiple skeletal lesions.
5. Laboratory tests show a significantly elevated serum calcium level (3.46 mmol/L) and markedly increased PTH (1057, normal range 10-60), indicating hyperparathyroidism.
6. Postoperative follow-up images demonstrate varying degrees of restorative changes in the lesions.
II. Possible Diagnoses
- Aneurysmal Bone Cyst (ABC)
Typically presents as an expansile lesion with hemorrhage and possible “fluid-fluid levels,” commonly seen in younger patients. However, it usually appears as a single lesion, and multiple lesions are less common. - Telangiectatic Osteosarcoma
This subtype of osteosarcoma can show partitioned cystic cavities and “fluid-fluid levels” similar to ABC, along with aggressive features. However, the patient’s bone scan findings of multiple lesions and elevated serum calcium are not typical for this diagnosis. - Giant Cell Tumor (GCT)
Often occurs in young adults after epiphyseal closure. It typically appears as an expansile lesion with lytic changes and can sometimes be confused with ABC or other malignancies. Pathology often shows abundant giant cells. - Brown Tumor
Secondary to hyperparathyroidism and relatively rare. Pathologically, it can show hemorrhage, giant cells, and fibrous tissue, and “fluid-fluid levels” can appear on imaging. It can present as multiple bone lesions, correlating with hypercalcemia and elevated PTH levels.
III. Final Diagnosis
Based on the patient’s age, clinical presentation (multiple lesions, persistent pain), laboratory results (significantly high serum calcium and elevated PTH), and postoperative clinical and imaging findings (lesion repair), the final diagnosis is “Brown Tumor due to Hyperparathyroidism.”
IV. Treatment Plan and Rehabilitation Program
1. Treatment Strategy
• Surgical Treatment: Surgical removal of the parathyroid adenoma is crucial. After the excision of a 5.3 g parathyroid adenoma, the patient’s serum calcium rapidly decreased, and the bone destruction from multiple brown tumors began to heal.
• Management of Fractures and Bone Lesions: In cases with a high risk of pathological fracture, surgical stabilization or internal fixation may be considered. If structural stability is not compromised or the risk of pathological fracture is low, bracing or splinting with regular follow-up may be sufficient.
• Medication: Postoperative calcium supplementation (to prevent hypocalcemia) and vitamin D may be considered to aid in bone remodeling.
2. Rehabilitation/Exercise Prescription
Given the bone destruction and the need for gradual recovery post-surgery, the following principles apply:
• Frequency: 3–5 sessions per week initially, depending on the patient’s tolerance.
• Intensity: Begin with low-intensity exercises, such as gentle range-of-motion and muscle-strengthening routines, then gradually increase resistance or load.
• Time: Start with 20–30 minutes per session; as endurance and bone condition improve, sessions can be extended to 45–60 minutes.
• Type: Emphasize safe, low-impact activities, such as aquatic exercises, seated or supine resistance training, and stability exercises.
• Progression: Increase load and range of motion based on improvements in joint mobility, pain levels, and bone density. If pain or discomfort occurs, adjust or pause the exercise program.
• Special Precautions: During the early postoperative period, avoid heavy loading and high-impact movements. Protect areas of bone fragility with braces or assistive devices to reduce fracture risk. If severe pain or functional impairment appears, consult a physician promptly.
V. Disclaimer
This report is a reference analysis based on the current clinical and imaging data and does not substitute for an in-person consultation or professional medical advice. Patients should seek timely consultation with a qualified medical institution or specialist for appropriate treatment and follow-up.
Human Doctor Final Diagnosis
Brown tumours